| Issue |
J Oral Med Oral Surg
Volume 29, Number 4, 2023
|
|
|---|---|---|
| Article Number | 44 | |
| Number of page(s) | 13 | |
| DOI | https://doi.org/10.1051/mbcb/2023039 | |
| Published online | 02 February 2024 | |
Systematic Review
Navigation in oral surgery: a systematic review
Department of Maxillofacial and Facial Plastic Surgery, Lyon Sud Hospital, Hospices Civils de Lyon, 165 Chemin du Grand Revoyet, 69495 Pierre-Bénite, Lyon, France
* Correspondence: alexis.oillic@gmail.com
Received:
7
July
2023
Accepted:
16
October
2023
Introduction: Dynamic navigation is a fast-growing technology in the field of head and neck surgery, which is now taking its place in oral surgery. The aim of this review was to present and describe all the uses of navigation in oral surgery. Materials and methods: A systematic review was conducted using all clinical trial/cases reports (Embase/PubMed) in which navigation is used during oral surgery, published over the last 5 yr. A total of 32 clinical trial/cases reports were analyzed. Results: Dynamic navigation was used in 7 different indications: implantology (55%), foreign body removal (15%), dental avulsion (12%), bone augmentation (9%), cellulitis (3%), benign tumour (3%), pre-prosthetic surgery (3%). A total of 335 patients were treated, 631 implants, 8 foreign bodies, 1 benign tumour, 24 dental avulsions, 3 bone augmentations, 1 cellulitis, and 1 pre-prosthetic surgery were found. In implantology, there were 500 standard implants, 75 zygomatic implants, 31 pterygoid implants, 1 short implant and 24 angulated implants. Conclusion: This review showed the recent development of dynamic navigation in oral surgery. The most common indication is dental implantology and few others indications seemed promising. This technique broadened its scope and might become an indispensable tool that can be used in many situations, increasing safety and predictability of a lot of procedure.
Key words: Dynamic navigation / oral surgery / computer-guided surgery
© The authors, 2024
 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
The advent of digital technology made virtual surgical planning (VSP) an everyday tool. Surgical planning software are a powerful diagnostic tool, they allow the anticipation of potential problems and facilitate communication with patients and colleagues. It is thus possible to perform the surgery almost completely in advance, without the patient, on planning software such as BlueSkyPlan®, CoDiagnostix®, DTX®, ProPlan® etc. Once the planning is validated by the operator and the patient, it remains a challenge to transfer the VSP to the operating room (OR). Several methods already exist, such as the design of computer-assisted static guides that can be 3D printed, through protocols commonly called CAD/CAM (computer assisted-design/computer assisted-manufactured). These techniques are widely documented in the literature and have multiple indications, well-described accuracy, known advantages and shortcomings [1]. This work will focus on surgical navigation, a dynamic guidance method that appeared in the field about 20 yr ago; and will try to understand its applications and its place in the field. In oral surgery, the accuracy of surgical navigation is most often assessed in implantology and it is compared with freehand implant surgery and statically guided implant surgery. The recently published review by Parra-Tressera et al. 2021 [2] showed a better accuracy of navigation on implant placement compared to the freehand technique and a similar accuracy to static guides [3,4].
However, the literature is limited, most of the reviews focus on single implantology case, due a lack of scientific data [2,5]. A systematic review was conducted of the last 5 yr, with the aim of overlooking the different applications available in oral surgery. This review described all the indications, results and calibration techniques of oral surgery that used navigation. The hypothesis is that the recent development of dynamic navigation in oral surgery broadened its scope and is becoming an indispensable tool that can be used in different indications.
Materials and methods
Search strategy and eligibility criteria
Were searched, all studies, about patient who underwent an oral surgical procedure, using a dynamic navigation, published between April 2017 and May 2022.
The databases MedLine by Pubmed and Embase were investigated at two periods of time, with a 4 months interval (April and July 2022). The searched terms were: “navigation”, “jaw”, “mandibular”, and “maxilla”, “zygomatic implant”, “pterygoid implant”, “dental implant”, “tooth extraction”, “foreign body”, “orthodontics”. The PubMed equations were: (navigation AND zygomatic implant) OR (navigation AND pterygoid implant) OR (Navigation AND dental implant) OR (navigation AND tooth extraction) OR (navigation AND foreign body) OR (navigation AND jaw) OR (navigation AND mandibular) OR (navigation AND maxilla) OR (navigation AND orthodontics) AND ((y_5 [Filter]) AND (casereports [Filter] OR clinicalstudy [Filter] OR clinicaltrial [Filter] OR comparativestudy [Filter] OR controledclinicaltrial [Filter])).
Study design and literature screening
The data were compared using the Population, Intervention, Comparison, Outcomes (PICO) criteria, were kept only articles about patients/population in need of an oral procedure, dynamic navigation was used each time, controlled or not and with results properly described.
The records and data were collected by a single reviewer. The selection criteria, the primary and secondary outcomes were described in Tables I and II.
The surgical indications were categorized according to the initial diagnosis and the treatment received; their distribution were expressed as percentages. The navigation systems used were also expressed as percentages; when it was not specified in the study, it was expressed in the final calculation as not reported (NR) The results of the surgeries were reported according to the initial surgical indication. The reflector used were classified according to their support (bone, dental, skin...) and whether they were invasive or not. The calibration methods were classified according to the types of fiducial markers (invasive or not).
Only the imaging used for real time navigation were collected; the imaging related to the diagnosis were not. The accuracy was related to implantology, it was described by 4 parameters: the coronal deviation (millimeters, mm), the apical deviation (mm), the angular deviation (degrees °), and the depth deviation (mm), missing data were not reported. The duration of the surgeries were compared according to the surgical indication; missing data were reported as NR.
Inclusion/Exclusion criteria.
Evaluation criteria.
Data extraction and method of analysis
The search was run in 4 phases and is documented in the flowchart presented in Figure 1.
 |
Fig. 1 Flowchart. |
Identification phase
The total numbers of recorded extracted articles was 166. Sixteen duplicated articles were eliminated.
Screening phase
The abstracts of the remaining 150 articles were examined based on our review questions and 112 articles were excluded. Only 38 articles remained.
Eligibility phase
After full text reading, 6 articles were excluded due to the confusion of some authors between “computer navigation” and “computer-guided (static guidance)”, or because they were comparative studies of dynamic navigation versus static guides.
Inclusion phase
The remaining 32 articles were included, and analyzed by the reviewer. Those articles represent a total of 335 patients who had undergone oral surgery in the past 5 yr.
Level of evidence and bias assessment
The level of evidence for each article selected was determined based on the concept outlined by the Oxford Centre for Evidence-Based Medicine (CEBM).
Revised Cochrane risk-of-bias tool for randomized trials (RoB 2) [6] was used for the assessment of quality of randomized clinical trials (RCTs) and the Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) instrument [7] was used for non-randomized controlled trials (NRCTs).
Results
The type of the included studies, their characteristics and their level of evidence are presented in Table III.
Risk of bias ranged from low to high with a high risk for the vast majority of included studies, especially concerning bias due to confounding or deviations from intended interventions. Detailed results of risk of bias assessment are presented in Tables IV–VI. This high risk of bias illustrate the versatility of the studies and could be a limitation of this current review.
A total of 7 main surgery indications were find regarding the use of navigation in oral surgery (Fig. 2).
The characteristics of the surgeries performed on the 335 patients are presented in Table VII.
No meta-analysis was performed because most of the data came from cases reports.
Review of the selected studies. AI: Angled implant/All on X: Implant-supported prosthetic rehabilitation with immediate loading on X implant/CC: Clinical case/FB: Foreign body/KOC: Keratinized odontogenic cyst/NR: Not reported/NC: No complication/NCT: Non-conservable tooth/PI: Pterygoid implant /PCS: Prospective clinical study/RCS: Retrospective clinical study/RCT: randomized clinical trial/SI: Standard implant /ShI: Short implant /SIOI: Surface in mm2 of the implant-bone interface/ZI: Zygomatic implant.
Quality assessment of each included study using the Cochrane ROBIN-I (Non randomised studies).
Risk of bias summary for the included studies using the Cochrane ROBIN-I.
Risk of bias assessment for the included studies using the Cochrane Risk of Bias Tool 2 (Randomized studies).
 |
Fig. 2 Distribution of indications found in oral surgery. |
Outcomes of the interventions.
Primary evaluation criteria
Indications, outcomes
Implantology
This review showed that the use of navigation in implantology is prominent, representing 19 articles (55%). A total of 631 implants were placed; short implant [8], pterygoid implant [9] and zygomatic implants [10–14]. The indications were varied; rehabilitation of the edentulous jaw using immediate implant loading with fixed prothesis, extraction-implantation, single implant in aesthetic zone [10,11,15–17], single implant with immediate loading in aesthetic zone [18] or the placement of standard minimally invasive implants (flapless) [19]. This review also found that navigation was used in the rehabilitation of carcinological sequelae by zygomatic implants (epithesis or maxillofacial prosthesis) [12,14]. The authors displayed a wide variety of techniques, which allowed for less invasive approaches in potentially irradiated patients, at risk of osteoradionecrosis [12,14]. Pellegrino et al. [11] described a technique comparable to a first drill guide for zygomatic implants, where a piezotome was used with a diamond insert that allowed a pre-drilling on the alveolar ridge and the zygomatic bone, without sliding on the bone surfaces. This technique allowed the passage of the drill and the implant in a non-guided way, avoiding a potential significant angular deviation on a 30 to 50 mm long implant. Pellegrino et al. [20] also described a technique where navigation permitted to prepare the site of implantation using a piezotome to perform a selective osteotomy, allowing the preparation of the different bone zones (cortical and trabecular bone). A benefit of navigation described by Stefanelli et al. [9] on pterygoid implant placement was that no loss of tactile sensation occurred during the drilling (in comparison with static guide). This is very valuable on implants of this type due to the low bone marrow density of the tuberosity.
Foreign body removal
This review found 5 studies (15%) using navigation in foreign body removal [13,22–24,37]. Two studies [23,25] described a technique that used resin mouthpieces, incorporated with radiological fiducial markers (for calibration), to allow mandibular blocking with the aim to limit anatomical differences related to mandibular dynamics, during surgery and imaging (muscular or cellulosic tissues causing migrations). On anatomical areas that are complex to access, some authors recommended to use endoscopes associated with navigation, to perform minimally invasive approaches.
Dental avulsion
A total of 4 articles (12%) of the reviewed studies were about navigation in the dental avulsion indication. When using navigation, Wang et al. [27] found no difference in their controlled preclinical study regarding avulsion of supernumerary teeth on operative time, unnecessary bone trauma, and position of supernumerary teeth. Pellegrino et al. [28] described a technique for the avulsion of impacted mandibular wisdom teeth without a flap (flapless); no postoperative painkiller was required.
Bone augmentation
The literature on bone augmentation associated with navigation is very limited. No clinical trial was found, only 3 case reports (9%). In one case, navigation was used for segmental rotation osteotomies [29]; the aim was to limit the damage of the inferior alveolar nerve. For that indication, the use of a system that integrates the piezotome was mandatory. Another case was a sinus augmentation with crestal approach (Summers technique) using Densah® drills that was performed using navigation [30]. The third case was the use of navigation to delineate graft areas and facilitate anatomical recognition to manage an alveolar cleft [31].
Cellulitis
The navigation was used by Han et al. [26] in abscess drainage (after 2 failures of conventional abscess drainage) on patient with deep abscess in the pterygomandibular space.
Benign tumours
Hong YP et al. [36] justified the use of navigation in surgical enucleation to get a safer surgery and to have a more complete curettage, especially with keratinized odontogenic cyst (KOC), which has a high recurrence rate. They described no recurrence within 2 yr follow-up.
Pre-prosthetic surgery
Magic et al. [17] used navigation to perform a bone reduction; the location of the reduction was decided according to a virtual wax-up and the smile line position.
Navigation systems
All the surgeries were perform using 12 systems, listed in Table VIII. The BrainLab© brand is the most used (30%).
Systems of navigation.
Calibration technique and nature of reflector
The patient reflector was non-invasive in 20 articles (62.5%), invasive in 7 articles (21.9%), both (mixed) in 3 articles (9.4%) and not indicated in 2 articles (6.2%). In the non-invasive reflectors and mixed (23 articles), the brackets were dental supported in 11 articles (47.8%), 9 were skin supported (39.1%) and 3 were implant anchored (13.1%). The implant supports were categorized as non-invasive because they were freehand implants that were an integral part of the treatment plan. All invasive reflectors are bone anchored (100%). Calibration was performed using fiducial markers that were non-invasive in 21 articles (65.6%), invasive in 6 articles (18.8%), mixed in 2 articles (6.2%), and NR in 3 articles (9.4%). Fiducials markers were radiological in 22 articles (68.7%) and anatomical in 7 articles (21.9%).
Some authors used extra oral bone anchorage (parietal bone, mastoid, zygomatic arch, supraorbital) to fix the fiducial markers in the edentulous and did not describe any complication [12,15].
Secondary primary evaluation
Duration of surgery
In implantology, only 3 articles mentioned the duration of surgery. Meng et al. [34] described an average time of 81.9 min for placement of 4–6 maxillary implants with a relatively long calibration of 10–15 min. Stefanelli et al. [9] found a significant difference in surgical time for pterygoid implant placement compared to the control group, with an average of 9.3 min with the navigated technique versus 22.1 min freehand. Pellegrino et al. [35] reported an average surgical time of 33 min for standard implant placement with augmented reality headset. For foreign body removal, abscess drainage, 5 articles mentioned [21,22,24,–26] the duration of surgery, ranging from 33 min to 1 h and 55 min. Zhang et al. [23] reported that the duration of surgery was non-extended when navigation was used. For avulsions of impacted teeth, 2 articles [27,35] reported the duration of surgery, ranging from 10.7 min to 30 min. Pellegrino et al. [27] described surgical times of less than 20 min for the avulsion of 2 third mandibular lower molars.
On a serie of cases, Pellegrino et al. [33] described a potential time saving when using augmented reality headset associated with navigation, but further studies would be warranted to confirm this hypothesis.
Imaging
The imaging systems used in the studies for dynamic navigation are Cone Beam Computed-Tomography (CBCT), 87.5%, and Computer tomography (CT) scan, 12.5%.
Complementary means
Some authors used the complementary tools; endoscopes in 3 cases [23,26,36], used for foreign body removal, benign tumour lesions or deep abscess drainage. In one case an augmented reality headset was used in [33], associated with standard implantology.
Types of anesthesia
Local anesthesia was the most common technique, used in 56.3% of cases. General anesthesia was used in 37.5% of the cases and the remaining 6.2% were the so-called “mixed” cases; a local anesthesia was performed for the placement of radiological markers and reflectors (the day before), followed by a general anesthesia for the placement of implants.
Accuracy
Navigation accuracy was only assessed in implantology. Only 2 articles were randomized controlled studies with the conventional technique (freehand) and navigation. Stefanelli et al. and Aydemir et al. found a significant difference between the navigated and freehand technique, with a better accuracy for navigation (Tab. IX).
Accuracy of navigation in implantology [coronal deviation (mm), apical deviation (mm), angular deviation (°) and depth deviation (mm)].
Follow-up and complications
Follow-up times ranged from no follow-up to 3 yr. Only 5 articles reported complications [12,15,18,25,27]. A total of 6/631 implants (0.05%) were lost due to failure of osseointegration. Wang et al. [27] described 2 complications for the navigated group, one early (1 hematoma), and one late (1 root hypoplasia). Bensing et al. [25] described a resolving lingual hypoesthesia following the removal of a foreign body located in the lingual floor.
Discussion
This review showed that the use of navigation in oral surgery had 7 different indications: implantology, foreign body removal, dental avulsion, benign tumour, bone augmentation, cellulitis and pre-prosthetic surgery. A total of 55% of the articles described a use related to implantology. There were an increasing number of articles about navigation as 43% of the articles were published in 2021–2022, compared to 15% in 2017–2018, which might show the growth of the use of this technology.
Few limits were discussed by the authors, even though all the foreign bodies were removed successfully, some authors described a difference between endoscopic vision and imaging [26]. They explained the potential inaccuracies by the difference in patient position during the acquisition of the imaging (standing) and during the surgery (lying down); it should be discussed to perform a CT scan or CBCT, lying down, like during the future procedure. They also explained the potential inaccuracies by the potential migration of the foreign body in soft tissues. To limit the movement of the foreign body during the removal surgery, the authors recommended to wait for fibrous encapsulation (3 to 6 weeks). It might decrease the discrepancies between imaging and per-op situation due to the gravity-related localization (soft tissues, sinus). Another limitation of the technology is that the guidance is based on a static and old image (its quality and the type of acquisition). All space modifications of our tissues shape will not be visible in preoperative or perioperative, as well as the migration of a foreign body. The use of imaging techniques only allows the visualization of radiopaque foreign bodies. These limitations are frequently discussed [21–24].
The calibration, as well as the fixation of the reflector are problematic for the edentulous jaw (absence of dental anatomical markers, or adjustable thermoformed bracket). Calibration is frequently performed using bone-anchored radiological markers. This implies the placement of bone anchored screws using local anesthesia (an additional procedure) with a postoperative CBCT or integrated into the final procedure (but requiring the realization of a per-operative CBCT), lengthening the procedure and complicating the management when a general anesthesia is performed. Fixing the reflector (bone anchor) on site can limit the implant positions and be cumbersome [10]. The nature of reflectors and fiducial markers can be different, which implies advantages and disadvantages. The skin as a reflector support or fiducial marker (surface calibration) was reported as a source of inaccuracy [22] compared to point calibration; as the skin is a depressible and mobile surface. Moreover, although it was not observed, the risk of skin-supported reflector eschar on long procedures (>2h), is mentioned by Sato et al. [22]. However, this protocol is still widely used in dynamic navigation for implantology, for the removal of foreign bodies or dental avulsions as it is very simple to use, with a rapid, non-invasive and less radiating calibration. The initial diagnostic imaging is sufficient, it seems interesting to recall that surface calibration (skin) is still used in neurosurgery, in systems such as BrainLab© or Medtronic [40].
The reflector support most used herein is dental tissue, it seems to be the preferred support, when it is possible (dentate patient) and proposed by the system. It can also be used as a support for radiological fiducial markers (calibration by points). However, the choice of teeth, without temporary prosthetic care (for the thermoformed bracket) or without periodontal damage leading to mobility, remains essential [15]. Dental elements are more and more used as anatomical fiducial markers, called dental surface calibration. Surface calibration (dental and bone), also called “trace registration” [32] are technologies about to save operative time, by avoiding to use thermoplastic brackets and to perform a 2nd imaging for a point calibration using radiological markers [8].
Bone tissue for reflector support and invasive X-ray fiducial marker support remains the most reliable solution [15]. Nevertheless, the placement of these markers sometimes requires complex planning [17] in order to optimize their distribution and to avoid collision; the collision may occur with planned implants, noble anatomical areas or areas where the anchorage could be potentially weak and therefore mobile (anterior wall of the sinus). These markers are similar to the planning of bone anchorage screw in static guidance.
The presence of a learning curve is described almost systematically; due to navigation the surgeon has an indirect vision, which may seem counter-intuitive. The authors described learning threshold, but the results were very different even for the experienced operator. Meng et al. reported that 5 cases were enough to reach the threshold [34], whereas, Stefanelli et al. [32] observed a better precision of the last 50 implants placed compared to the first 50. This result may suggest that the threshold of progression is not necessarily reached as quickly.
As already said, general anesthesia was performed in 37.5% of the cases, which could be problematic as CBCT could not be performed intraoperatively when placement of radiological fiducial markers is necessary, thus, it must be done beforehand.
Hong YP et al. [36] in addition to the use of navigation during the surgery to perform enucleation of a KOC, performed a chemical enucleation using 80% ethanol (for the first time as well), therefore, a strong confusion bias exists.
Pellegrino et al. [28] study about minimal invasive wisdom teeth removal remains uncontrolled, a split-mouth design should be considered on a larger number of patients.
In all articles reviewed the duration of surgery using navigation was described in only 32%. It appeared that the data are slightly contradictory, the differences being explained by the variety of the surgeries in this review and of the systems used.
A majority of articles were case reports (71%), whose scientific value is questionable, more clinical trial are needed in these specific indications. Many surgeries were founding to be successful with aid of dynamic navigation but according to the low level of evidence and high level of bias of many articles, the results should be interpreted with caution.
Perspective
In addition to the versatility found of this technology, Wang et al. described the navigation as a potential educational tool to address the lack of experience of young surgeons [27,35] in complex dental avulsions; the parallel in oral implantology could easily be made. The navigation could be interesting for autogenous bone block harvesting (ramus, chin, and parietal) in order to limit the damages to nearby anatomical elements; no article in this review described this use. Stefanelli et al. [10] mentioned the possibility to use anatomical bone fiducial markers with surface calibration, which could be of great use for the edentulous in implantology, because the current protocol is often complex and time-consuming.
There is different systems of navigation and many systems are dedicated to implantology (ImplaNav/X-Guide/NaviDent), which testifies the orientation of navigation in oral surgery. Meng et al. [34] described the importance of having a system dedicated to an indication, to save time during the different steps (specific planning integrated in the software, calibrations). The absence of a navigation system integrating endoscopy was highlighted by Zhang et al. [23].
Moreover, it seemed it might be a successful surgical tool to help in the surgery of patients with deep abscess; when it is difficult to accurately target the abscess due to inflammation or trismus [26].
Conclusion
The indications of navigation in oral surgery are already multiple and surgical navigation systems are dedicated to some of these indications, such as implantology, the most common. As navigation co-exists with other technologies, its evolution will depend on their improvement, such as artificial intelligence. It is an essential basis for augmented surgery, or even passive and active robotic surgery. In the view of this work, further studies should focus on one of those specifics indications with controlled clinical trial to measure the clinical relevance of this technology.
Conflict of interest
None reported.
Funding
The author did not receive any funding for this article.
Ethical approval
Ethical Approval was not required.
Informed consent
This study did not require informed consent.
Authors contributions
A.Oillic: Investigation, Methodology, Writing original draft; A. Varazzani, A. Carlier: Supervision, Reviewing.
Abbreviations
All on X: Implant-supported prosthetic rehabilitation with immediate loading on X implant
CBCT: Cone Beam Computed-Tomography
KOC: Keratinized odontogenic cyst
PCS: Prospective clinical study
RCS: Retrospective clinical study
RCT: randomized clinical trial
SIOI: Surface in mm2 of the implant-bone interface
References
- Block MS, Emery RW. Static or dynamic navigation for implant placement—choosing the method of guidance. J Oral Maxillofac Surg 2016;74:269–277. [CrossRef] [PubMed] [Google Scholar]
- Parra-Tresserra A, Marquès-Guasch J, Ortega-Martínez J, Basilio-Monné J, Hernández-Alfaro F. Current state of dynamic surgery. A literature review. Med Oral 2021;e576–e581. [Google Scholar]
- Kaewsiri D, Panmekiate S, Subbalekha K, Mattheos N, Pimkhaokham A. The accuracy of static vs. dynamic computer‐assisted implant surgery in single tooth space: a randomized controlled trial. Clin Oral Impl Res 2019; clr. 13435. [Google Scholar]
- Block MS, Emery RW, Cullum DR, Sheikh A. Implant placement is more accurate using dynamic navigation. J Oral Maxillofac Surg 2017;75:1377–1386. [CrossRef] [PubMed] [Google Scholar]
- Gargallo-Albiol J, Barootchi S, Salomó-Coll O, Wang H lay. Advantages and disadvantages of implant navigation surgery. A systematic review. Ann Anat Anatomischer Anz 2019;225:1–10. [CrossRef] [Google Scholar]
- Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;l4898. [Google Scholar]
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;i4919. [Google Scholar]
- Pellegrino G, Lizio G, Rossi F, Tuci L, Ferraioli L, Stefanelli LV, et al. A 4 mm-long implant rehabilitation in the posterior maxilla with dynamic navigation technology: a case report after a three-years post-loading follow-up. Int J Environ Res Public Health 2021;18:9808. [CrossRef] [PubMed] [Google Scholar]
- Stefanelli LV, Graziani U, Pranno N, Di Carlo S, Mandelaris GA. Accuracy of dynamic navigation surgery in the placement of pterygoid implants. Int J Periodontics Restorative Dent 2020;40:825–834. [CrossRef] [PubMed] [Google Scholar]
- Lopes A, Nobre MA, Santos D. The workflow of a new dynamic navigation system for the insertion of dental implants in the rehabilitation of edentulous jaws: report of two cases. J Clin Med [Internet 2020;9. Disponible sur: https://www.embase.com/search/results?subaction=viewrecord&id=L2003722691&from=export [Google Scholar]
- Pellegrino G, Tarsitano A, Taraschi V, Vercellotti T, Marchetti C. Simplifying zygomatic implant site preparation using ultrasonic navigation: a technical note. Int J Oral Maxillofac Implants 2018;33:e67–e71. [CrossRef] [PubMed] [Google Scholar]
- Tso TV, Chao D, Tanner J, Freymiller EG, Jayanetti J. Prosthetic reconstruction of a patient with an irradiated total rhinectomy with navigated surgical placement of a single zygomatic implant: a clinical report. J Prosthet Dent 2021;125:352–356. [CrossRef] [PubMed] [Google Scholar]
- Wang F, Bornstein MM, Hung K, Fan S, Chen X, Huang W, et al. Application of real-time surgical navigation for zygomatic implant insertion in patients with severely atrophic maxilla. J Oral Maxillofac Surg 2018;76:80–87. [CrossRef] [PubMed] [Google Scholar]
- Zhou W, Fan S, Wang F, Huang W, Jamjoom FZ, Wu Y. A novel extraoral registration method for a dynamic navigation system guiding zygomatic implant placement in patients with maxillectomy defects. Int J Oral Maxillofac Surg 2021;50:116–120. [CrossRef] [PubMed] [Google Scholar]
- Stefanelli LV, Mandelaris GA, Franchina A, Pranno N, Pagliarulo M, Cera F, et al. Accuracy of dynamic navigation system workflow for implant supported full arch prosthesis: a case series. Int J Environ Res Public Health 2020;17:E5038. [CrossRef] [PubMed] [Google Scholar]
- Wang M, Eitan M, Zhan Y, Shen H, Liu F. Digital workflow for prosthetically driven implant navigation surgery in a fully edentulous patient: a case report. Int J Comput Dent 2021;24:303–315. [PubMed] [Google Scholar]
- Magic M, Wang F, Fan S, Wu Y. Dynamic navigation guidance for bone reduction in maxilla: case report. Int J Oral Maxillofac Implants 2021;36:Ie1–Ie6. [CrossRef] [Google Scholar]
- Pozzi A, Arcuri L, Carosi P, Nardi A, Kan J. Clinical and radiological outcomes of novel digital workflow and dynamic navigation for single‐implant immediate loading in aesthetic zone: 1‐year prospective case series. Clin Oral Implants Res 2021;32:1397–1410. [CrossRef] [PubMed] [Google Scholar]
- Pellegrino G, Taraschi V, Andrea Z, Ferri A, Marchetti C. Dynamic navigation: a prospective clinical trial to evaluate the accuracy of implant placement. Int J Comput Dent 2019;22:139–147. [PubMed] [Google Scholar]
- Pellegrino G, Taraschi V, Vercellotti T, Ben-Nissan B, Marchetti C. Three-dimensional implant positioning with a piezosurgery implant site preparation technique and an intraoral surgical navigation system: case report. Int J Oral Maxillofac Implants 2017;32:e163–e165. [CrossRef] [PubMed] [Google Scholar]
- Wang H, Yang CY, Li Z. Traumatic displacement of teeth into maxillary sinus and the retrieval assisted by computer-assisted navigation: a case report. Medicine (Baltimore) 2018;97:e13865. [CrossRef] [PubMed] [Google Scholar]
- Sato H, Shiogama S, Narihira K, Chikuda J, Nakamura S, Abe Y, et al. Removal of small foreign bodies from the maxillary sinus using CT image-guided surgical navigation and rapid paired-point registration and calibration with reference markers on an occlusal splint. Oral Maxillofac Surg Cases [Internet 2019;5. Disponible sur: https://www.embase.com/search/results?subaction=viewrecord&id=L2001426983&from=export [Google Scholar]
- Zhang C, Wu J, Yang C, Liu N, Hui W, Zhang Y, et al. New solutions to improve the accuracy of the navigation-guided foreign body removal in craniomaxillofacial deep space. J Craniofac Surg 2020;31:e577–e580. [CrossRef] [PubMed] [Google Scholar]
- Chen S, Liu YH, Gao X, Yang CY, Li Z. Computer-assisted navigation for removal of the foreign body in the lower jaw with a mandible reference frame: a case report. Medicine (Baltimore) 2020;99:e18875. [CrossRef] [PubMed] [Google Scholar]
- Bensing JR, McElroy KE, Perez L. Retrieval of displaced third molar into the sublingual space using 3-dimensional navigation assistance. J Oral Maxillofac Surg 2021;79: 537.e1–537.e7. [CrossRef] [PubMed] [Google Scholar]
- Han SM, Chae HS, Lee HN, Jeon HJ, Bong JP, Kim JH. Computed tomography-guided navigation assisted drainage for inaccessible deep neck abscess: a case report. Medicine (Baltimore). mars 2019;98:e14674. [CrossRef] [PubMed] [Google Scholar]
- Wang J, Zhang W, Wu SS, Guo CB, Cui NH. Navigation in bone-impacted premaxillary supernumerary tooth removal: a preliminary clinical trial. Int J Comput Dent 2021;24:363–374. [PubMed] [Google Scholar]
- Pellegrino G, Lizio G, Ferri A, Marchetti C. Flapless and bone-preserving extraction of partially impacted mandibular third molars with dynamic navigation technology. A report of three cases. Int J Comput Dent 2021;24:253–262. [PubMed] [Google Scholar]
- Felice P, Bonifazi L, Karaban M, Berti C, Pellegrino G, Barausse C. Dynamic navigated « Sandwich » technique: a novel surgical approach for safe osteotomies in the rehabilitation of an atrophic posterior mandible: a case report. Methods Protoc 2021;4:34. [CrossRef] [PubMed] [Google Scholar]
- Jain S, Solanki A. A dynamic surgical navigational approach for immediate implantation and transcrestal sinus augmentation. J Indian Soc Periodontol 2021;25:451–456. [CrossRef] [PubMed] [Google Scholar]
- Zhang Y, Dai J, Fu X, Yang J, Fu Y, Li J. Real-time image-guided navigation in the management of alveolar cleft repair. Cleft Palate-Craniofac J [Internet 2021; ((Zhang Y; Dai J; Fu X; Li J., lijian_hubei@whu.edu.cn) The State Key Laboratory Breeding Base of Basic Science of Stomatology (Hubei-MOST) and Key Laboratory of Oral Biomedicine Ministry of Education, School and Hospital of Stomatology, Wuhan University, Wuhan, China). Disponible sur: https://www.embase.com/search/results?subaction=viewrecord&id=L2014218258&from=export [Google Scholar]
- Stefanelli LV, DeGroot BS, Lipton DI, Mandelaris GA. Accuracy of a dynamic dental implant navigation system in a private practice. Int J Oral Maxillofac Implants 2019;34:205–213. [CrossRef] [PubMed] [Google Scholar]
- Pellegrino G, Mangano C, Mangano R, Ferri A, Taraschi V, Marchetti C. Augmented reality for dental implantology: a pilot clinical report of two cases. BMC Oral Health 2019;19:158. [CrossRef] [PubMed] [Google Scholar]
- Meng T, Zhang X. Accuracy of intentionally tilted implant placement in the maxilla using dynamic navigation: a retrospective clinical analysis. Int J Oral Maxillofac Surg 2022;51:552–557. [CrossRef] [PubMed] [Google Scholar]
- Wang J, Cui NH, Guo YJ, Zhang W. Navigation-guided extraction of impacted supernumerary teeth: a case report. J Oral Maxillofac Surg 2017;75: 1136.e1–1136. e5. [CrossRef] [Google Scholar]
- Hong YP, Kim CS. Intraoperative CT image-guided navigation system-assisted endoscopic enucleation of a mandibular odontogenic Keratocyst. Ear Nose Throat J 2019;98:NP144–NP146. [CrossRef] [PubMed] [Google Scholar]
- Sukegawa S, Yoneda S, Kanno T, Tohmori H, Furuki Y. Optical surgical navigation-assisted removal of a foreign body using a splint to simplify the registration process: a case report. J Med Case Rep 2019;13:209. [CrossRef] [PubMed] [Google Scholar]
- Aydemir CA, Arısan V. Accuracy of dental implant placement via dynamic navigation or the freehand method: a split-mouth randomized controlled clinical trial. Clin Oral Implants Res 2020;31:255–263. [CrossRef] [PubMed] [Google Scholar]
- Wei SM, Shi JY, Qiao SC, Zhang X, Lai HC, Zhang XM. Accuracy and primary stability of tapered or straight implants placed into fresh extraction socket using dynamic navigation: a randomized controlled clinical trial. Clin Oral Investig 2022;26:2733–2741. [CrossRef] [PubMed] [Google Scholar]
- Duque S, Gorrepati R, Kesavabhotla K, Huang C, Boockvar J. Endoscopic endonasal transphenoidal surgery using the BrainLAB® headband for navigation without rigid fixation. J Neurol Surg A Cent Eur Neurosurg 2013;75:267–269. [CrossRef] [PubMed] [Google Scholar]
All Tables
Review of the selected studies. AI: Angled implant/All on X: Implant-supported prosthetic rehabilitation with immediate loading on X implant/CC: Clinical case/FB: Foreign body/KOC: Keratinized odontogenic cyst/NR: Not reported/NC: No complication/NCT: Non-conservable tooth/PI: Pterygoid implant /PCS: Prospective clinical study/RCS: Retrospective clinical study/RCT: randomized clinical trial/SI: Standard implant /ShI: Short implant /SIOI: Surface in mm2 of the implant-bone interface/ZI: Zygomatic implant.
Quality assessment of each included study using the Cochrane ROBIN-I (Non randomised studies).
Risk of bias assessment for the included studies using the Cochrane Risk of Bias Tool 2 (Randomized studies).
Accuracy of navigation in implantology [coronal deviation (mm), apical deviation (mm), angular deviation (°) and depth deviation (mm)].
All Figures
 |
Fig. 1 Flowchart. |
| In the text | |
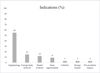 |
Fig. 2 Distribution of indications found in oral surgery. |
| In the text | |
Current usage metrics show cumulative count of Article Views (full-text article views including HTML views, PDF and ePub downloads, according to the available data) and Abstracts Views on Vision4Press platform.
Data correspond to usage on the plateform after 2015. The current usage metrics is available 48-96 hours after online publication and is updated daily on week days.
Initial download of the metrics may take a while.


