| Issue |
J Oral Med Oral Surg
Volume 24, Number 1, January 2018
|
|
|---|---|---|
| Page(s) | 29 - 32 | |
| Section | Cas clinique / Short case report | |
| DOI | https://doi.org/10.1051/mbcb/2017020 | |
| Published online | 25 May 2018 | |
Short Case Report
Peripheral osteoma of the mandibular crest: a short case study
1
Oral Surgeon (DESCO), Department of Oral Surgery, Dental Service at the Hôpital Bretonneau− AP-HP, Faculty of Medicine Paris XII-UPEC,
Paris, France
2
Faculty of Dentistry, Université Paris Descartes, Hôpital Bretonneau AP-HP Lab EA2496,
Paris, France
3
Doctor of Medicine, Pathologist,
Paris, France
4
MCU-PH Paris-Descartes, Department of Oral Surgery, Dental Service at the Hôpital Bretonneau− AP-HP,
Paris, France
* Correspondence: arthurfourcade@me.com
Received:
26
June
2017
Accepted:
4
September
2017
Introduction: Osteoma is a benign slow-growing osteogenic neoplasm characterized by the proliferation of cancellous and/or cortical bone. Jaw bones are seldom affected. Observation: We observed a rare case of a patient with a peripheral mandibular osteoma, which was surgically removed. Comments: Frequently asymptomatic, a peripheral osteoma looks like a bony swelling that may be sessile or pedunculated. Imaging examinations show a well-circumscribed radio-opaque mass. Symptomatic osteomas must be surgically excised and submitted for histological evaluation. Conclusion: Excessive osseous healing following a tooth extraction may explain this rare form of osteoma.
Key words: osteoma / peripheral / mandible
© The authors, 2018
 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Osteoma is a benign osseous lesion characterized by the proliferation of cancellous and/or cortical bone [1]. It can be peripheral, central, or extraskeletal [1,2]. The etiology is not well known [2], and osteomas of the jaw are relatively rare [2,3].
Observations
A 41-year-old patient of Caucasian origin without any significant medical history presented with a mass located in the retromolar region of the right mandible. Its appearance followed an avulsion of the right mandibular wisdom tooth performed 2 years earlier. There were no postoperative complications after this procedure. According to the patient, the lesion gradually increased in size over 2 years. The patient described the lesion as “annoying” while eating but painless.
The intraoral examination showed that this protrusion was approximately 1.5 × 1 cm and had a pedunculated base at the junction between the crest and the rising branch of the mandible (Fig. 1). The lesion was immobile and had a hard consistency. It was covered with a whitish hyperkeratotic attached gingiva. Inflammatory signs were absent on the lesion and around the lesion. The remainder of the intraoral and extraoral examination was unremarkable with, in particular, the absence of lingual and labiomental hypoesthesia.
The orthopantomogram showed a radio-opaque trabecular corticalized growth (Fig. 2). Three-dimensional imaging (cone beam computed tomography; CBCT) has helped to clarify the structure of the lesion (Fig. 3). It appeared to be confined to the bone and pedunculated on the lingual slope of the right mandibular crest.
Because of the atypical localization of the lesion, its continued growth and the inconvenience to the patient, a complete resection of the lesion was proposed.
Local anesthesia was administered using injections of mepivacaine (Scandicaine) and adrenaline 1/100 000. A mucoperiosteal incision was made with a scalpel blade no. 15 starting on the distal side of tooth 47 and continuing toward the crestal lesion. The incision was then passed through its upper pole and stretched back over the rising mandibular ramus. This permitted the removal of the bony protrusion with the help of a periosteal stripper. Prolonged dissection on the vestibular and lingual aspects of the mandible made it possible to visualize the lesion pedicel (Fig. 4). The bony lesion was resected at the base of its pedicle, using a fine-ball cutter mounted on a handpiece under saline irrigation. As a result, the bony crest was smoothened. Throughout the procedure, the lingual nerve was carefully protected by placing a malleable plate between the lingual cortical version and the periosteum in relation to the lesion. The excess fibromucosal tissue surrounding the lesion was then resected with a cold blade (Fig. 4). After a betadine wash, the site was sutured without tension with interrupted absorbable sutures (Vicryl® 3/0).
The resected specimen including the attached fibromucosal tissue was sent to the pathology laboratory for histological analysis (Fig. 5). Postoperatively, the patient was prescribed a level-1 analgesic (1 g of paracetamol in case of pain) and chlorhexidine mouthwashes (3 times a day) for 5 days.
The histological analysis revealed a benign, well-differentiated osseous lesion (Fig. 6). It had trabecular lamellar bone at the center with hard cortical bone surrounding it. It was covered with a dense, fibrous capsule with a slightly increased cellularity. Stellate cells were observed toward the osseous lesion under a hyperplastic, parakeratotic squamous epithelium. A few lymphocyte or plasmocyte clusters were observed. These results confirmed the diagnosis of cortical spongy osteoma covered by slightly hyperplastic squamous epithelium.
The surgical procedure was completed without complications and the postoperative follow-up at D15 showed complete mucosal healing.
 |
Fig. 1 Intraoral view: pedunculated retromolar swelling, covered by a hyperkeratotic gingiva. |
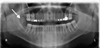 |
Fig. 2 Panoramic X-ray: solitary pedunculated osteoma, well-defined, appearing as a radio-opaque mass in the right retromolar area. |
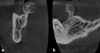 |
Fig. 3 CBCT: tumor with lingual pedicle on the right mandibular ridge, osseous density with a border of condensation. a: frontal section. b: sagittal section. |
 |
Fig. 4 Intraoperative view a: isolated osteoma. b: mucosal membrane. |
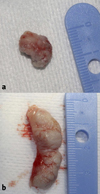 |
Fig. 5 Operative samples. a: osseous, 1.5 × 1 cm. b: mucosal. |
 |
Fig. 6 Histopathological analysis (hematoxylin-eosin stain). a: magnification ×25: trabecular lamellar central bone (on the left side of the picture, arrows shows the trabecular bone) with peripheral cortical bone covered by a chorion (on the right side of the picture). b: magnification ×100: peripheral cortical bone. |
Comments
An osteoma is a benign, slow-growing, painless bone tumor characterized by the proliferation of mature spongy and/or compact bone covered with periosteum [1]. There are three variants that differ depending on their location:
-
Peripheral osteomas: They are found on the periosteum and present themselves as hard masses; they can be sessile or pedunculated and are attached to the cortical bone.
-
Central osteomas: They are much rarer and are found on the endosteum (thin layer of connective tissue lining the surface of the medullary cavity of the long bones); they are located within the bones.
-
Extraskeletal osteomas: They develop in soft tissues, most frequently within muscles [1,2,4].
Peripheral osteomas are the most common. They are usually located on long bones such as the femur or the radius. At the maxillofacial level, the frontal, ethmoid and maxillary bones are the most frequently affected [1–4]. More rarely, peripheral osteomas are found in the jaw [1–4]. In the mandible, where they are usually located on the outer side, they occur more commonly at the angle, the lower edge, and the condyles [1,2,4].
They are more common in young adults and are twice as common in men as in women [1–4]. They usually appear in adolescence and can gradually increase in size by up to several centimeters.
Often asymptomatic and incidentally discovered on a routine X-ray examination, they can, depending on their volume and location, lead to discomfort, pain, facial asymmetry, headaches, occlusal dysfunction, a limitation of mandibular motion, or, more rarely, paresthesia due to nerve compression [1–5].
In imaging examinations, they appear as a rounded or oval, well-circumscribed, radio-opaque lesions attached to the affected cortical bone by a wide base or a pedicle [2,5]. CT scans are the best method for examining the area for a more precise preoperative evaluation of the lesion border and its relationship with adjacent anatomical structures [1,2,5].
Their etiology has not yet been clearly identified. The etiology is thought to be congenital (residue of the embryological periosteum), neoplastic, and reactive. In the case of reactive osteomas, trauma or infection would be the cause of a periosteal lifting (by a hematoma or edema), which would induce an osteogenic reaction maintained by opposing muscular forces [1–5]. The most probable etiology in this patient was an excess of bone healing in response to the avulsion of tooth 48.
A conservative method is recommended in most cases of osteomas. Surgical resection, initially intraoral, or even extraoral, may be indicated in some cases [1–5] when the osteoma causes functional or aesthetic discomfort, pain, traumatic ulcers, or periodontal disorders. The choice of a resection must also take into account the potential risks related to the surrounding anatomical structures (nerves and blood vessels).
The resected specimen must be systematically examined in a histological examination. Usually, the lesion consists of cortical (lamellar), spongy (trabecular) or mixed bone. Its composition is similar to that of mature bone [1,2,4].
Several differential diagnoses must be considered [1,2]:
-
a simple exostosis (torus), often bilateral and symmetrical, in a zone of attached gingiva whose growth stops at puberty; it is histological identical to osteomas;
-
an osteoblastoma, which is defined as a lesion attached to the cortical bone; it is painful and fast growing;
-
an osteoid osteoma, which is also a painful lesion that often shows rapid growth;
-
an osteochondroma, which usually has a condylar or coronoid location on the mandible;
-
an advanced stage of ossifying fibroma, conventionally combining a fibrous component within a cemento-osseous formation;
-
a complex odontoma whose radiographic opacity is close to that of a tooth.
Recurrences are rare and malignant transformation has never been described in the literature [1–4].
Multiple osteomas of the jaws are frequently associated with Gardner syndrome (autosomal dominant disease) [1–5]. In case of multiple lesions, the other signs associated with this syndrome, i.e., digestive polyps (possible malignant evolution), cutaneous tumors, exostosis of the skull, and supernumerary teeth, should be investigated.
Conclusion
A peripheral osteoma is a secondary onset lesion. The present case appears to be a reactive osteoma because of excessive bone healing following a tooth extraction. The clinical and radiological examination makes it possible to arrive at a diagnosis and decide on the right surgical indication. A histological examination confirms the diagnosis and the benign nature of the lesion. Although recurrences are rare and a malignant transformation has never been described, long-term, clinical, and possibly radiological monitoring is recommended.
Conflicts of interests
The authors declare that they have no conflicts of interest in relation to this article.
References
- Geron ABG, Carvalho VA, dos Santos JL, et al. Surgical management of traumatic peripheral osteoma of the mandible. J Craniofac Surg 2017;28:405–408. [CrossRef] [Google Scholar]
- Sayan NB, Uumlccedilok C, Karasu HA, et al. Peripheral osteoma of the oral and maxillofacial region : a study of 35 new cases. J Oral Maxillofac Surg 2002;60:1299–1301. [CrossRef] [PubMed] [Google Scholar]
- Kaplan I, Calderon S, Buchner A. Peripheral osteoma of the mandible: a study of 10 new cases and analysis of the literature. J Oral Maxillofac Surg 1994;52:467–470. [CrossRef] [PubMed] [Google Scholar]
- Woldenberg Y, Nash M, Bodner L. Peripheral osteoma of the maxillofacial region. Diagnosis and management: a study of 14 cases. Med Oral Patol Oral Cir Bucal 2005;10:139–142. [Google Scholar]
- Kashima K, Rahman OI, Sakoda S. Unusual peripheral osteoma of the mandible: report of 2 cases. J Oral Maxillofac Surg 2000;58:911–913. [CrossRef] [PubMed] [Google Scholar]
All Figures
 |
Fig. 1 Intraoral view: pedunculated retromolar swelling, covered by a hyperkeratotic gingiva. |
| In the text | |
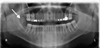 |
Fig. 2 Panoramic X-ray: solitary pedunculated osteoma, well-defined, appearing as a radio-opaque mass in the right retromolar area. |
| In the text | |
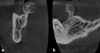 |
Fig. 3 CBCT: tumor with lingual pedicle on the right mandibular ridge, osseous density with a border of condensation. a: frontal section. b: sagittal section. |
| In the text | |
 |
Fig. 4 Intraoperative view a: isolated osteoma. b: mucosal membrane. |
| In the text | |
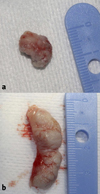 |
Fig. 5 Operative samples. a: osseous, 1.5 × 1 cm. b: mucosal. |
| In the text | |
 |
Fig. 6 Histopathological analysis (hematoxylin-eosin stain). a: magnification ×25: trabecular lamellar central bone (on the left side of the picture, arrows shows the trabecular bone) with peripheral cortical bone covered by a chorion (on the right side of the picture). b: magnification ×100: peripheral cortical bone. |
| In the text | |
Current usage metrics show cumulative count of Article Views (full-text article views including HTML views, PDF and ePub downloads, according to the available data) and Abstracts Views on Vision4Press platform.
Data correspond to usage on the plateform after 2015. The current usage metrics is available 48-96 hours after online publication and is updated daily on week days.
Initial download of the metrics may take a while.


