| Issue |
J Oral Med Oral Surg
Volume 31, Number 3, 2025
|
|
|---|---|---|
| Article Number | 21 | |
| Number of page(s) | 6 | |
| DOI | https://doi.org/10.1051/mbcb/2025021 | |
| Published online | 18 July 2025 | |
Case Report
Custom-made subperiosteal implants for atrophic maxilla rehabilitation: a digital approach
Department of Maxillofacial and Facial Plastic Surgery, Lyon Sud Hospital, Hospices Civils de Lyon, 165 Chemin du Grand Revoyet, 69495 Pierre-Bénite, Lyon, France
* Correspondence: t.lechene@orange.fr
Received:
6
February
2025
Accepted:
12
March
2025
Introduction: Full-arch reconstruction with dental implants is considered the gold standard for dental rehabilitation. However, in cases of advanced maxillary atrophy, the placement of conventional implants may be unfeasible. Such situations can be managed using zygomatic implants or, alternatively, by placing subperiosteal implants. Observation: A 74-year-old completely edentulous woman with severe maxillary atrophy was treated using two subperiosteal implants. A provisional prosthesis was delivered 48 hours after the surgical procedure. Conclusion: Subperiosteal implant placement appears to be an effective alternative to zygomatic implants for the rehabilitation of the atrophic maxilla. This has been made feasible by the development of patient-specific virtual planning protocols.
Key words: Subperiosteal implants / maxillary atrophy / digital workflow / virtual planning / immediate loading
© The authors, 2025
 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
The rehabilitation of the atrophic maxilla remains a challenge for oral surgeons. Traditional approaches, combining sinus augmentation with guided bone regeneration, have proven effective but involve lengthy treatment times, invasive procedures, and greater financial cost for patients. Moreover, these techniques carry the risk of partial or total graft failure [1,2]. Vertical ridge augmentation procedures, which are essential for restoring adequate bone height for implant placement, are highly technique-sensitive and carry a risk of complications. A systematic review reported an overall complication rate of 16.9% for vertical ridge augmentation, increasing to 23.9% when using bone block graft [3].
Graftless techniques have been developed, with zygomatic implants at the forefront. While their success is well documented in the literature, these approaches are not without complications and technical challenges [4,5].
In recent years, a previously unpopular method—subperiosteal implants— has returned to practice, particularly with the advent of imaging software (CBCT) combined with computer-aided design and manufacturing techniques [6–8].
Historically, subperiosteal dental implants were originally introduced in the 1940s as a viable solution for patients with severe alveolar ridge atrophy, offering an alternative when conventional endosteal implants were not viable. Early designs, however, faced considerable limitations due to the limitations of the manufacturing techniques and imaging methods of the time. The lost-wax casting process frequently resulted in imprecise fittings and structural inaccuracies, while invasive bone impression procedures and suboptimal materials, such as cobalt-chromium alloys prone to corrosion and adverse tissue reactions led to high infection rates and low long-term success. These technical and biological shortcomings eventually led to a decline in their use, especially as Dr Branemark's pioneering work on osseointegration marked the beginning of the era of endosteal implants [6,9,10].
Recent technological advancements have, however, renewed interest of subperiosteal implants. Modern diagnostic tools such as computed tomography (CT) and cone-beam CT (CBCT) now allow for precise, non-invasive mapping of the jawbone anatomy, while CAD-CAM design and additive manufacturing techniques (including direct metal laser sintering) enable the production of highly customised, accurate implants. Additionally, improved materials such as titanium and its alloys have enhanced biocompatibility and osseointegration, significantly reducing complications and invasiveness. Together, these innovations have transformed subperiosteal implants into a promising, less invasive alternative for rehabilitating patients with significant bone loss [6–8,11].
This article presents a case of atrophic maxilla rehabilitation using custom-made subperiosteal implants as an alternative to zygomatic implants, with a one-year follow-up. Oral consent was obtained.
Observation
A 74-year-old female patient was referred for fixed implant rehabilitation of the maxilla and mandible. She had no significant medical history. In the maxilla, she presented with a mobile bridge supported by six implants. In the mandible, five implants were exposed in the oral cavity. A panoramic radiograph revealed peri-implantitis affecting the implants. (Fig. 1).
The first step involved the removal of the maxillary and mandibular implants, followed by the fabrication of adapted complete removable prostheses. Three months later, an evaluation was performed, including dual CT scans (patient scan with the prosthesis in place and scan of the prosthesis alone) and photographs taken with and without the prostheses in place.
The radiological assessment revealed a maxillary atrophy classified as Cawood class 6 [12]. Initially, we considered rehabilitation using four zygomatic implants. However, during planning (Blue Sky Plan software ®), we identified a very thin residual bone thickness beneath the nasal floor in the area of the anterior right zygomatic implant (0.74 mm), which posing risks of oro-nasal communication and peri implant mucosal dehiscence. Moreover, we have identified a maxillo-zygomatic anatomy classified as ZAGA 4 [13], which implies an extra sinus implant placement with anchorage being ensured solely by the zygoma (Fig. 2).
We proposed a maxillary rehabilitation solution using subperiosteal implants to optimally address both bone and prosthetic constraints. Two custom-made subperiosteal implants (AMSJI) were designed in collaboration with the CADskills laboratory® using the patient's DICOM and STL data. Each of these implants featured five screw holes in the maxilla, each associated with three multi-unit prosthetic connectors (Fig. 3).
Surgery was performed under general anesthesia. The first step involved raising a full-thickness flap using a crestal incision and two distal retrotuberosal releasing incisions. The bone was then thoroughly exposed to facilitate placement of the custom-made subperiosteal implants according to the patient's anatomy. One of the main challenges was ensuring a precise fit between the implants and the bone, as minor bone interference, likely due to residual biomaterial from a previous bone graft, complicated the procedure. Both implants were fixed to the maxilla using self-tapping screws (diameter of 2.3 mm and length from 7 mm to 15 mm), and 4-0 Vicryl sutures were placed around the pillars (Fig. 4). Bichat's fat pad was used to isolate the implants from oral cavity and to prevent from dehiscence of peri implant soft tissues.
The flap closure around the implants did not require any releasing incisions.
A digital impression was taken using four scan bodies like an All-on-4 procedure, the final two multi-unit abutments was used for the definitive prosthesis. A screw retained provisional prosthesis was loaded on four abutments 48 hours later.
Postoperative instructions included a mixed and soft diet for three months. The treatment regimen comprised 7 days of amoxicillin (3 g/day), 3 days of corticosteroids (60 mg per day), and 10 days of chlorhexidine mouth rinses (three times per day).
Six months later, the definitive prostheses were delivered. In the meantime, four mandibular implants had been placed without complication. No soft tissue dehiscence or implant loosening was observed (Fig. 5).
One-year post-surgery, no soft tissue changes or implant mobility were observed. The definitive prosthesis remained in place, and the patient reported being satisfied both functionally and aesthetically. (Fig. 6).
 |
Fig. 1 (A) Clinical Situation (B) Radiological situation. |
 |
Fig. 2 Zygomatic Implant Planning (A) Digital avatar and implant planning (B) Subnasal bone reserve. |
 |
Fig. 3 Subperiosteal implants on the printed model. |
 |
Fig. 4 Intraoperative Procedure (A) Subperiosteal implants in place with the flap raised (B) Mucosa closed over the multi-unit abutments. |
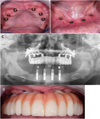 |
Fig. 5 Clinical and radiological situation at 6 months: (A) Maxilla view(B) Mandibular view (C) Panoramic radiograph (D) Maxilla with the provisional prosthesis. |
 |
Fig. 6 (A) Definitive prosthesis (B) Front picture. |
Commentary
Subperiosteal implants remained unpopular for a long time, primarily due to the complexity of the manufacturing techniques—which required two surgical interventions—along with high postoperative infection rates and challenges in prosthetic loading [6,9,10]. However, advances in 3D radiological data acquisition (CBCT/DICOM), combined with implant-design software and laser-based additive manufacturing (CAD/CAM), have enabled the renewed interest of subperiosteal implants as a potential technique for rehabilitating an atrophic maxilla [6].
In their systematic review, Anitua et al. reported an implant survival rate of 97.8% at 21 months [14]. These implants allow for the functional loading of a prosthesis. Radiographic evaluation of bone remodeling after additively manufactured subperiosteal jaw implantation (AMSJI) did not exhibit significant alveolar ridge atrophy. However it could be detected beneath the fixation wings [15]. AMSJI's monobloc structure contributes to reduced micromovement at the bone-implant interface. By eliminating multiple connections and ensuring a seamless design, this approach limits micromovements and fosters bone ingrowth, ultimately improving long-term osteointegration and durability. To assess its mechanical performance, AMSJI has been validated using finite element analysis [16].
The literature indicates also reports, high patient satisfaction and a significant improvement in oral health [17]. The most commonly reported complications are hardware exposure in the oral cavity and mobility; however, these issues rarely affect implant survival [18,19].
However, significant limitations remain. According to Herce López et al. The literature reveals that data on subperiosteal implants are still scarce and primarily based on short-term follow-up case series and retrospective studies, making it difficult to draw robust long-term conclusions. Common complications include soft tissue dehiscence leading to implant exposure and other mechanical issues, such as fractures of provisional prostheses. While these complications do not appear to compromise short-term implant survival, their potential long-term effects, especially regarding peri-implantitis and overall implant stability are still uncertain [20].
In comparison, zygomatic implants, a widely documented rehabilitation technique with reported implant success rates of 96% at 6 years according to ITI (international team for implantology) consensus report of 2023 [4] remain a treatment of choice for rehabilitating the atrophic maxilla. However, complications have been reported, most notably maxillary sinusitis in 14.2% of cases [4]. This approach also allows for immediate prosthetic loading [5]. This treatment approach is considered complex and is not always feasible, as it depends on the volume and density of the zygomatic bone. Moreover, although rare, the risk of orbital floor involvement remains a serious complication requiring advanced surgical expertise and meticulous planning [21].
A 2025 retrospective study compared zygomatic implants with subperiosteal implants over a five-year period, assessing implant survival, soft tissue management, and postoperative complications. The study included 150 patients, with zygomatic implants evaluated for immediate functional loading and sinus-related complications, while subperiosteal implants were assessed for their customised design and soft tissue integration. Results showed comparable survival rates (zygomatic: 96.3%, subperiosteal: 97.1%, p = 0.278). However, zygomatic implants had a higher incidence of sinus-related complications (12.4%) and potential orbital damage, whereas subperiosteal implants had fewer cases of peri-implantitis (5.6%, p < 0.05). Procedural duration was shorter for zygomatic implants (177 min vs. 123 min), making them a more time-efficient option. However, subperiosteal implants allowed for re-implantation after failure, offering flexibility unavailable with zygomatic implants. Soft tissue stability was superior in subperiosteal implants, reducing the risk of soft tissue complications. Additionally, zygomatic implants, being mass-produced, had lower manufacturing costs compared to the 3D-printed, custom-designed subperiosteal implants. The study concluded that zygomatic implants are advantageous for immediate loading and shorter procedural times but require advanced surgical expertise. In contrast, subperiosteal implants offer a safer, customisable alternative, particularly in anatomically complex cases, highlighting the importance of individualised treatment planning [22]. To our knowledge, there are no other articles comparing subperiosteal implants to another rehabilitation technique.
While this case report provides valuable insights into the use of custom-made subperiosteal implants for maxillary rehabilitation, it presents inherent scientific limitations. As a single-case study, it lacks the statistical power and generalisability of larger cohort studies or randomised controlled trials. The absence of a control group makes it difficult to compare the effectiveness of subperiosteal implants with alternative treatments, such as zygomatic implants, in a standardised manner. Additionally, the follow-up period of one year, though promising, is insufficient to assess long-term implant survival, potential complications, and bone remodeling processes over time. Further research, including multi-center studies with larger sample sizes and extended follow-up durations, is necessary to confirm the reliability, safety, and long-term outcomes of this technique.
Conclusion
The rehabilitation of atrophic maxillae with custom-made subperiosteal implants appears to be an effective and predictable technique, largely due to advancements in digital technologies. This method may represent a valuable alternative to zygomatic implants, which remain technically demanding are associated with a range of complications. However, further long-term clinical studies are necessary to validate the efficacy and stability of this treatment approach.
Funding
This research did not receive any specific funding.
Conflicts of interest
The authors declare no conflict of interests.
Data availability statement
All data generated or analysed during this study are included in this published article.
Author contribution statement
Thomas Le Chêne : writing, editing; Alexis OILLIC: main operator, supervision, reviewing. Sébastien Duffort : reviewing.
Ethics approval
Ethical approval was not required.
References
- Tolstunov L, Hamrick JFE, Broumand V, Shilo D, Rachmiel A. Bone augmentation techniques for horizontal and vertical alveolar ridge deficiency in oral implantology. Oral Maxillofac Surg Clin North Am 2019;31:163–191. [Google Scholar]
- Buser D, Urban I, Monje A, Kunrath MF, Dahlin C. Guided bone regeneration in implant dentistry: Basic principle, progress over 35 years, and recent research activities. Periodontol 2000 2023;93:9–25. [Google Scholar]
- Urban IA, Montero E, Amerio E, Palombo D, Monje A. Techniques on vertical ridge augmentation: Indications and effectiveness. Periodontol 2000 2023;93:153–182. [Google Scholar]
- Al-Nawas B, Aghaloo T, Aparicio C, Bedrossian E, Brecht L, Brennand-Roper M, et al. ITI consensus report on zygomatic implants: Indications, evaluation of surgical techniques and long-term treatment outcomes. Int J Implant Dent 2023;9:28. [Google Scholar]
- Polido WD, Machado-Fernandez A, Lin WS, Aghaloo T. Indications for zygomatic implants: A systematic review. Int J Implant Dent 2023;9:17. [Google Scholar]
- Łoginoff J, Majos A, Elgalal M. The evolution of custom subperiosteal implants for treatment of partial or complete edentulism in patients with severe alveolar ridge atrophy. J Clin Med 2024;13:3582. [Google Scholar]
- Strappa EM, Memè L, Cerea M, Roy M, Bambini F. Custom-made additively manufactured subperiosteal implant. Minerva Dent Oral Sci 2022;71:353–360. [Google Scholar]
- Mommaerts MY. Evolutionary steps in the design and biofunctionalisation of the additively manufactured sub-periosteal jaw implant AMSJI for the maxilla. Int J Oral Maxillofac Surg 2019;48:108–114. [Google Scholar]
- Weinberg BD. Subperiosteal implantation of a vitallium (cobalt-chromium alloy) artificial abutment. J Am Dent Assoc 1950;40:549–562. [Google Scholar]
- Dantas TA, Vaz P, Samuel FS. Subperiosteal dental implants: Past or future? A critical review on clinical trials/case reports and future directions. J Dent Implants 2023;13:35. [Google Scholar]
- Vatteroni E, Covani U, Menchini Fabris GB. The new generation of subperiosteal implants for patient-specific treatment of atrophic dental arches: Literature review and two case reports. Int J Periodontics Restorative Dent 2023;43:735–741. [Google Scholar]
- Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg 1988;17:232–236. [Google Scholar]
- Aparicio C. A proposed classification for zygomatic implant patient based on the zygoma anatomy guided approach (ZAGA): A cross-sectional survey. Eur J Oral Implantol 2011;4:269–275. [Google Scholar]
- Anitua E, Eguia A, Staudigl C, Alkhraisat MH. Clinical performance of additively manufactured subperiosteal implants: A systematic review. Int J Implant Dent 2024;10:4. [Google Scholar]
- Van den Borre C, Rinaldi M, De Neef B, Loomans NAJ, Nout E, Van Doorne L, et al. Radiographic evaluation of bone remodeling after additively manufactured subperiosteal jaw implantation (AMSJI) in the maxilla: A one-year follow-up study. J Clin Med 2021;10:3542. [Google Scholar]
- De Moor E, Huys SEF, Van Lenthe GH, Mommaerts MY, Vander Sloten J. Mechanical evaluation of a patient-specific additively manufactured subperiosteal jaw implant (AMSJI) using finite-element analysis. Int J Oral Maxillofac Surg 2022;51:405–411. [Google Scholar]
- VVan den Borre C, De Neef B, Loomans NAJ, Rinaldi M, Nout E, Bouvry P, et al. Patient satisfaction and impact on oral health after maxillary rehabilitation using a personalised additively manufactured subperiosteal jaw implant (AMSJI). J Pers Med 2023;13:297. [Google Scholar]
- Dimitroulis G, Gupta B, Wilson I, Hart C. The atrophic edentulous alveolus. A preliminary study on a new generation of subperiosteal implants. Oral Maxillofac Surg 2023;27:69–78. [Google Scholar]
- Korn P, Gellrich NC, Spalthoff S, Jehn P, Eckstein F, Lentge F, et al. Managing the severely atrophic maxilla: Farewell to zygomatic implants and extensive augmentations? J Stomatol Oral Maxillofac Surg 2022;123:562–565. [Google Scholar]
- Herce-López J, Pingarrón M del C, Tofé-Povedano Á, García-Arana L, Espino-Segura-Illa M, Sieira-Gil R, et al. Customised subperiosteal implants for the rehabilitation of atrophic jaws: A consensus report and literature review. Biomimetics (Basel) 2024;9:61. [Google Scholar]
- Weber MI, Koschitzki E. Ocular complications of zygomatic dental implants: A systematic review. Cureus 2024;16:e67535. [Google Scholar]
- Zielinski R, Okulski J, Piechaczek M, Łoś J, Sowiński J, Sadowska-Sowińska M, et al. Five-year comparative study of zygomatic and subperiosteal implants: Clinical outcomes, complications, and treatment strategies for severe maxillary atrophy. J Clin Med 2025;14:661. [Google Scholar]
Cite this article as: Le Chêne T, Duffort S, Oillic A. 2025. Custom-made subperiosteal implants for atrophic maxilla rehabilitation: a digital approach. J Oral Med Oral Surg. 31, 21: https://doi.org/10.1051/mbcb/2025021
All Figures
 |
Fig. 1 (A) Clinical Situation (B) Radiological situation. |
| In the text | |
 |
Fig. 2 Zygomatic Implant Planning (A) Digital avatar and implant planning (B) Subnasal bone reserve. |
| In the text | |
 |
Fig. 3 Subperiosteal implants on the printed model. |
| In the text | |
 |
Fig. 4 Intraoperative Procedure (A) Subperiosteal implants in place with the flap raised (B) Mucosa closed over the multi-unit abutments. |
| In the text | |
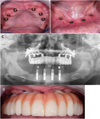 |
Fig. 5 Clinical and radiological situation at 6 months: (A) Maxilla view(B) Mandibular view (C) Panoramic radiograph (D) Maxilla with the provisional prosthesis. |
| In the text | |
 |
Fig. 6 (A) Definitive prosthesis (B) Front picture. |
| In the text | |
Current usage metrics show cumulative count of Article Views (full-text article views including HTML views, PDF and ePub downloads, according to the available data) and Abstracts Views on Vision4Press platform.
Data correspond to usage on the plateform after 2015. The current usage metrics is available 48-96 hours after online publication and is updated daily on week days.
Initial download of the metrics may take a while.


