| Issue |
Med Buccale Chir Buccale
Volume 23, Number 4, December 2017
|
|
|---|---|---|
| Page(s) | 190 - 191 | |
| Section | Cas clinique / Short case report | |
| DOI | https://doi.org/10.1051/mbcb/2017022 | |
| Published online | 12 December 2017 | |
Short Case Report
Canalicular adenoma of the upper lip: a short case study
1
Centre Massilien de la Face,
Marseille, France
2
Service d'Odontologie, CHU Timone,
Marseille, France
* Correspondence: ugo.ordioni@gmail.com
Received:
22
July
2017
Accepted:
8
September
2017
Introduction: Canalicular adenoma (CA) is a benign tumor that develops in the accessory salivary glands. Observation: We reported a case of CA of the upper lip in a 61-year-old man. Discussion: The clinical diagnosis of CA is difficult, and a lot of possible differential diagnoses exist, including benign or malignant salivary tumors. Thus, the diagnosis may be challenging and must rely on histological examination findings. The treatment is surgical in nature and the prognosis is excellent.
Key words: salivary glands / salivary gland neoplasms / adenoma / lip
© The authors, 2017
 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Observations
A 61-year-old man consulted for a lesion of the upper lip which had appeared over the course of 2 years. He was asthmatic, and he was under treatment with nasal beclomethasone dipropionate spray and bilastin.
There was no functional pain or signs. A clinical examination revealed a mucosal nodule of 1.5 cm from the upper left lip (Fig. 1). The nodule was hard in consistency and was mobile. The mucous membrane covering the lesion was normal. There was no associated lymphadenopathy.
The lesion was resected under local anesthesia. Macroscopically, the tumor was well demarcated and was yellowish in color. A histological examination carried out in the operating room showed a CA with epithelial proliferation, which was organized in canals and in septa, consisting of regular tall cylindrical cells without any cellular atypia. The stroma was loose and fibrohyaline in nature. Immunohistochemistry (AE1-AE3) emphasized epithelial proliferation (Fig. 2). The tumor was negative for P63. No recurrence was identified in the 3 months after resection.
 |
Fig. 1 Clinical aspect of the lesion. |
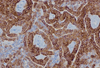 |
Fig. 2 Microscopic aspect of the lesion. Double row of high cylindrical cells forming cords. Intense expression of pancytokeratin (AE1/AE3). |
Discussion
CA is a benign tumor of the salivary glands. It is in terms of frequency, it is the third-most common salivary gland tumor after, pleomorphic adenoma and mucoepidermoid carcinoma [1]. However, it is still rare and represents 1% of all salivary tumors and 4% of the tumors affecting the accessory salivary glands [2]. Its peak incidence is in the seventh decade of life. The average age of occurrence is 65 years, and it is not frequently found in patients aged <50 years. There has never been a case in a child [1]. The sex ratio (F/M) is 1.8:8 [2].
It is most frequently located on the upper lip (80% CA cases). The buccal mucosa is more rarely affected (9.25% of tumors). The major salivary glands are very rarely affected. Multiple cases of CA have been described [3].
Clinically, CA occurs as an asymptomatic mucosal nodule that rarely exceeds 2 cm in size. The overlying mucosa is normal and not ulcerated, but it can sometimes have a bluish color [2]. Their growth is slow.
Macroscopically, the tumor is well demarcated and may or may not be encapsulated, and may have a lumpy appearance. The classical histological description shows a double row of cylindrical cells forming cords in a loose stroma (Fig. 2). These double rows are tight or separate forming canaliculi with a tree-like appearance, or cysts or channels when the section is perpendicular. The cells are in usually cylindrical but can also be cuboidal, and the number of mitoses is low. The stroma is paucicellular and rich in blood capillaries. Immunohistochemistry shows positivity for anti-cytokeratin, anti-vimentin, and anti-S100 antibodies and negativity for smooth actin, calponin, P63, and E-cadherin [1]. In 9% of cases, the CA is multifocal [1,4].
Differential diagnosis is made with a mucoid cyst, vascular tumor, phleboliths, lipoma, or another salivary gland tumor, including basal cell adenoma, low-grade adenocarcinoma, and cystic adenoid carcinoma. The distinction between these salivary gland tumors and multifocal CA can be difficult, the immunohistochemistry is useful for the diagnosis [4,5].
The treatment is always surgical in nature. The prognosis is good, and no malignant transformation has ever been described in the literature. Recurrences are rare but are more frequent in multifocal CA.
Conflicts of interests
The authors declare that they have no conflicts of interest in relation to this article.
References
- Thompson LDR, Bauer JL, Chiosea S, McHugh JB, Seethala RR, Miettinen M, Müller S. Canalicular adenoma: a clinicopathologic and immunohistochemical analysis of 67 cases with a review of the literature. Head Neck Pathol 2015;9:181–195. [CrossRef] [PubMed] [Google Scholar]
- Barnes L, Eveson J, Reichart P, Sidransky D. Pathology and genetics of tumors of the head and neck. World Health Organization classification of tumors, Lyon: IARC Press, 2001. [Google Scholar]
- Tyralik D, Dzierwa-Gawron A, Ryś J. Canalicular adenoma of the upper lip. Metachronous (multifocal) canalicular adenoma of the upper lip: a case report of an unusual finding. Pol J Pathol 2013;64:71–74. [CrossRef] [PubMed] [Google Scholar]
- Samar ME, Avila RE, Fonseca IB, Anderson W, Fonseca GM, Cantín M. Multifocal canalicular adenoma of the minor labial salivary glands. Int J Clin Exp Pathol 2014;7:8205–8210. [PubMed] [Google Scholar]
- Sivolella S, Valente M, De Biagi M, Mazzoleni SS, Tellini E. Canalicular adenoma immunoprofile: a case report. Gerodontology 2014;31:320–324. [CrossRef] [PubMed] [Google Scholar]
All Figures
 |
Fig. 1 Clinical aspect of the lesion. |
| In the text | |
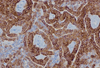 |
Fig. 2 Microscopic aspect of the lesion. Double row of high cylindrical cells forming cords. Intense expression of pancytokeratin (AE1/AE3). |
| In the text | |
Current usage metrics show cumulative count of Article Views (full-text article views including HTML views, PDF and ePub downloads, according to the available data) and Abstracts Views on Vision4Press platform.
Data correspond to usage on the plateform after 2015. The current usage metrics is available 48-96 hours after online publication and is updated daily on week days.
Initial download of the metrics may take a while.


