| Issue |
J Oral Med Oral Surg
Volume 30, Number 2, 2024
|
|
|---|---|---|
| Article Number | 12 | |
| Number of page(s) | 9 | |
| DOI | https://doi.org/10.1051/mbcb/2024014 | |
| Published online | 05 July 2024 | |
Original Research Article
Reducing the anxiety of adults during dental avulsions with virtual reality: a randomized controlled trial
Maxillofacial Surgery and Oral Surgery Department, CHU Caen, France
* Correspondence: anaisp20@hotmail.fr
Received:
28
January
2023
Accepted:
27
April
2024
Purpose: Dental anxiety is a recurring problem in the daily life of oral surgeons. The purpose of this study was to determine whether the use of virtual reality (VR) during dental avulsions can reduce anxiety in adults. Methods: This was a single centre randomized controlled clinical trial. Patients were randomized into two groups (with and without VR). VR experience was realized with music and visualization of 3D landscape thanks to a head-mounted display. Patients completed the State Trait Anxiety Inventory State (STAI-YA) and the Visual Analog anxiety Scale (VAS) before and after the intervention by transcribing the anxiety felt during this one. The main outcome was the evolution of STAI-YA score, a decrease of more than 8 points was sought. Secondary outcomes were studying the choice of the metric, defining the factors influencing the evolution of STAI-YA, studying side effects and the desire to repeat the experience. Results: 40% of patients in the VR group had a STAI-YA score reduced by more than 8 points between before and during the intervention compared to 20% in the control group. This result was significant (p = 0.026). VAS decreased by more than 2cm in 40% of patients in the VR group against 20% of patients in the control group. If a patient declared being afraid of the dentist, the VR seemed more efficient to reduce the anxiety. No side effects were observed, 96% of patients wanted to repeat the VR experience. Conclusion: VR appears to be effective in reducing the anxiety of adults during dental avulsions.
Key words: Oral surgery / virtual reality / anxiety
© The authors, 2024
 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
About 20% of patients are afraid of the dentist, of which 10% are phobic and, despite technical developments, this percentage remains the same [1,2]. The most anxiety element is the surgical intervention, regardless of the gender, age, ethnicity and basal level of anxiety of the patient [3]. Anxiety is multifactorial, specific to each individual, and is expressed differently [4]. This can be increased heart rate, faster respiration, faintness, dizziness, feelings of tightness or agitation. Concerning dental anxiety, its origin can be endogenous factors (heredity) but also exogenous factors such as personal traumatic experiences or reported by the entourage [4,5]. This fear can lead to the development of a vicious circle as described by Armfield et al.: patients delay or cancel their consultations; they consult when symptoms such as pain appear so they are having difficulty with the consultation, anxiety will increase and they will cancel futures appointments [6]. The phenomenon can have negative consequences on the oral health or even the general health of the patient. Interventions such as dental avulsions are performed under local anaesthesia most of the times, so we must deal with anxiety. Currently, medicinal methods are used in first intention. A few non-drug methods are also used as hypnosis, the broadcasting of audio and/or visual content.
For some years now, virtual reality (VR) is studied. It is a technique of immersing the patient in a pleasant environment through distraction. This non-pharmacological method permit to directing the person's attention to a harmless event by means of a stimulus (audio and visual) in the immediate environment [7]. The aim is blocking negative thoughts and reducing the unpleasant sensations. Rajeev et al. showed that sensations such as sight, vibrations, noises and smells contribute to anxiety and one of the advantages of virtual reality, unlike other audiovisual distractions, is that the patient's visual and auditory fields are covered by virtual information, preventing sensory input from the real dental world [8]. Different areas of health use VR, for example, Hoffman et al. has highlighted the effectiveness of VR in pain treatment during dressing changes or physical therapy in burn patients (adults and children) [9,10]. Hoffman et al. proved that depending on the sophistication of VR, the feeling of presence differs. Feeling of presence corresponds to the amount of attention of the patient towards the virtual information [11]. VR is also used in oncology, for pain management by combining it with morphine and for reducing anxiety before radiotherapy sessions or before skin cancer surgery [12–14].
In the field of oral surgery, a literature review conducted by López-Valverde et al. in 2020 showed that several randomized studies demonstrate that VR reduces the feeling of pain and anxiety during dental care or avulsion in children [15]. For adults, only three randomized studies were completed. Sweta et al. performed a randomized study that supported a decrease in pain, according to the Visual Analogue Scale (VAS), when using VR for anaesthesia before dental avulsions. Anxiety would also be lower when using VR, this was measured by comparing measures of hemodynamics (preoperative and postoperative oxygen saturation, intraoperative pulse rate); however, the sample is small (n = 50) [16]. Yamashita et al. studied the impact of VR during extraction of mandibular third molars. It showed a decrease in anxiety according to the VAS comparing the score before/during within the VR group while in the control group the score increased [17]; however the level of anxiety before the intervention is unknown. The last study is that of Mladenoviç et al. who studied the impact of VR during the extraction of mandibular third molars [18]. The patients were operated for the first time without VR, then during the second session, two weeks later, they benefited from VR. The results showed a decrease in pain assessed by the wong baker faces pain rating scale and a decrease in heart rate between before and during the intervention during the session with VR.
Faced with this limited number of studies carried out in an adult population which have various limitations, the purpose of this study was to carry out a randomized study on an adult population, in real conditions, during dental avulsions on maxilla or mandible, with teeth on arcade or included.
The evolution of anxiety during dental avulsions has been investigated by comparing a group with VR and another group without VR. The main outcome was to study the evolution of the State-Trait Anxiety Inventory (STAI-YA) score between before and during the intervention in the two groups.
Secondary outcomes were:
Study the comparability of the results with another metric to assess anxiety (VAS).
Study the factors influencing the evolution of the STAI-YA anxiety score.
Study the side effects of VR and the desire or not to repeat the VR experience.
Materials and methods
Study design
The study was prospective, randomized, and monocentric. Two groups were defined: VR group (VR+) versus control group (VR-). The patients in the test group benefited from virtual reality and the control group received no anxiolytics or other means of reducing anxiety.
The REVIDEN study (“Realité Virtuelle avulsions Dentaires”) was carried out in the oral surgery department of the university hospital center in Caen. It received the approval of a Committee for the Protection of Persons on 09/09/2021 and the RCB ID number was n°2021-A01969-32. Informed consent was obtained from all participants in this study. All methods were performed in accordance with relevant guidelines. The data was collected for 6 months, between November 2021 and May 2022. They were analyzed using computer methods respecting statistical and medical secrecy.
Adults who consulted for at least two dental extractions were recruited. The exclusion criteria were patients suffering of motion sickness, claustrophobia, uncontrolled epilepsy, visual impairment, hearing disability, non-French speakers, pregnant women, protected adults and people followed by a psychiatrist whether for depression, bipolarity, schizophrenia. The day of the intervention, patients who had consumed anxiolytics were excluded.
Subjective evaluation
The investigators hypothesize that more patients had a decrease greater than 8 points in the STAI-YA score between before and during the intervention in the VR group compared to the group without VR.
The State-Trait Anxiety Inventory (STAI) in its state anxiety part (-YA) was used to assess anxiety levels. It consisted of 20 self-assessment items numbered from 1 to 20 which were scored from 1 (not at all) to 4 (a lot). The overall score varied from 20 to 80, higher was the score, greater was the anxiety [19]. Spielberger (1983) created this scale sensitive to variation and reported that the average STAI-YA score for adults when under no stress was 35.7 for men and 35.2 for women [19]. Zemła et al. showed that preoperative anxiety was clinically present when scores reach at least 44 [20]. Thus, an increase in the score of more than 8.8 points (44–35.2 = 8.8) indicated the presence of anxiety. The objective was to reduce the STAI-YA score by more than 8 points.
Absolute delta STAI-YA:
Stai-ya (during) − Stai-ya (before) <−8 points.
The patients also transcribed anxiety felt on a visual analogue scale (VAS). It ranged from 0 cm (absence of anxiety) to 10 cm (maximum anxiety). The VAS decrease threshold was set at 2 cm because, in the literature, it was accepted that a difference of more than 2 cm (on a 10 cm scale) for this to be clinically relevant [21].
Absolute delta VAS:
VAS (during) − VAS (before) < −2 cm.
Implementation of the intervention
During the first session, when the patient had given his consent, the doctor asked him about his characteristics: age?, gender?, profession?, is this the first dental extraction under local anesthesia?, is this the first experience with VR?, tobacco consumption?, cannabis consumption?, daily consumption of anxiolytics?, medical history?, fear of the dentist?
During the second session, patients completed the STAI-YA and the VAS before and after the intervention by transcribing the anxiety felt during this one. Then, anesthesia, dental avulsions and sutures were performed in the same way in both groups. One surgeon operated on all the patients.
The presence of side effects was collected as well as the patient's desire or not to repeat the VR experience. If the patient reported symptoms such as nausea, vomiting, dizziness, headache, stomach pain, we suspected the presence of cybersickness. This phenomenon is due to the difference between visual information and motor information received by the vestibular system when using electronic devices.
VR experience
The head-mounted display was a PICO G2® on loan from HealthyMind®. Patients chose one or more landscapes from 6 choices (zen garden, walk in the woods, snowy mountain, paradise beach, scuba diving, sunny mountain). Each landscape lasted 20 minutes. It was quite possible to lengthen the session or shorten it during the intervention thanks to a tablet made available to the operator. The headphones were a wireless Bose® with Bluetooth connection, also on loan from HealthyMind®. The audio reproduced a soothing sound atmosphere and a specific medical speech for each theme with breathing exercises.
Data collection methods
A list with numbers from 1 to 120 was produced prior to the study on Excel. Each number was assigned a random group (with and without VR).
During the first consultation, the patient was assigned a number (the practitioner followed the list on Excel) and therefore a group. Both practitioner and patient knew the patient's group for the next appointment.
Upon completing the questionnaires at the second consultation, the patient indicated his assigned number instead of providing his name. Then, the practitioner filled in the Excel file with the data collected (characteristics of the patients, STAI-YA score, VAS), which were associated with the patient's number, and which were therefore anonymous.
Data analyses
Using the results obtained in a study using the STAI-YA scale in dermatological surgery and dental avulsion surgery [22], the average score on the STAI-YA scale was at least 35–40 in the control group. An effect considered to be clinically significant corresponded to a decrease of more than 8 points between before and during the procedure. If it considers that 50% of the patients will decrease by more than 8 points in the VR group and 30% in the control group, it takes for a risk α equal to 5% approximately 120 patients (60 people per group) for get 90% power.
The data was presented using standard parameters with, for each variable, the mean plus or minus one standard deviation (m±s) or the number and its percentage, n (%).
For the means, the comparative analysis used the Student's t test or the analysis of variance, a robust method, after verification of the equality of the variances by the Levene test. In case of doubt about normality and/or non-compliance with the hypothesis of equality of variances, the comparison was verified by the Mann–Whitney test.
For percentages, the chi-square test or Fisher's exact test were performed.
A multivariate analysis by logistic regression was carried out by including the variables presenting a degree of significance lower than 20% in univariate analysis according to a descending stepwise procedure.
All the analyzes were carried out bilaterally at the α risk equal to 5% with the software IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.
Results
Population
Flow chart
119 patients were initially included in the study, including 62 in the VR group and 57 in the control group. 9 patients were excluded since they did not come to the intervention (2 in the VR group and 7 in the control group) and 5 patients in the VR group were not analyzed because there were missing data. 55 patients were analyzed in the VR group and 50 in the control group (Fig. 1).
 |
Fig. 1 Flow chart. |
Description (Tab. I)
Gender: there were 26 women (47.3%) in the VR group and 22 women (44%) in the group without VR; there was no significant difference between the two groups.
Age: the mean age was 34.6 ± 15.9 years in the VR group, it was 43.7 ± 21.6 years in the group without VR; it was significantly higher in the VR group with p = 0.016.
History of dental extractions: there were significantly more patients whom it was their first tooth extraction in the VR group (31 or 56.4% against 18 or 36.0% in the VR group).
Virtual reality experience: the populations were comparable; the majority of patients had never experienced virtual reality before (34 patients in the control group (68.0%) and 31 patients in the VR group (56.4%)).
Addictions: the consumption of tobacco and cannabis was similar in the two groups. For tobacco there were 20 patients (40%) in the control group and 24 (43.6%) in the VR group and for cannabis respectively 3 (6.0%) and 4 (7.3%).
Anxiety: the number of patients who declared being afraid of the dentist was comparable in the two groups with 16 patients (32.0%) in the control group VR and 20 patients (36.4%) in the VR group. It was the same with the daily consumption of anxiolytics which concerns 3 patients (6%) in the control group and 2 (3.6%) in the VR group.
There was nevertheless a significant difference in the baseline STAI-YA score (before the intervention) between the two groups with an average of 39.8 ± 12.7 in the control group whereas it was higher in the VR group with an average of 45.0 ± 12.8.
Characteristics of patients.
The main outcome measures
22 patients in the VR group decreased their STAI-YA score of more than 8 points between before and during the intervention, i.e. 40% of the patients in this group. This result was significantly different from that of the control group where a decrease of more than 8 points only concerned 10 patients, i.e. 20% of the patients in this group, with p = 0.026 (Tab. II) (Fig. 2).
The recruited workforce being 105 instead of 120 as planned, an a posteriori power calculation was carried out. For α equal to 5% and 55 patients in the VR group versus 50 in the control group and 40% versus 20% respectively of patients who had a clinically significant reduction of more than 8 points on the STAI-YA, the power of the study was 85% (Fig. 3).
Distribution of groups according to significant absolute deltas.
 |
Fig. 2 Distribution of groups according to absolute deltas. % = percentage of individuals concerned. Absolute delta STAI-YA = Score STAI-YA (during) − Score STAI-YA (before). Absolute delta VAS = Score VAS (during) − score VAS (before). STAI-YA = State Trait Anxiety Inventory − State VAS = Visual analogue scale (anxiety). VR = Virtual reality. |
 |
Fig. 3 Power of the study as a function of sample size. |
Secondary outcomes
Analysis with VAS
22 patients had a VAS reduced by more than 2 cm between before and during the operation, i.e. 40% of patients in the VR group. This result was significantly different compared to the control group in which a decrease greater than 2 cm concerned only 8 patients, i.e. 16% of patients in this group with p = 0.009 and a power greater than 90% (Tab. II) (Fig. 2).
Factors influencing the evolution of the STAI-YA score
The analyses revealed factors influencing the reduction in the STAI-YA score, namely (Tab. III):
The inclusion group with VR.
Patients who reported being afraid of the dentist.
If a patient belonged to the VR group, he was 3 times more likely to decrease in the STAI-YA score by more than 8 points compared to a patient in the control group (OR 3 and p = 0.028).
A patient who reported being afraid of the dentist was 7.9 times more likely to decrease the STAI-YA score by more than 8 points compared to a patient who was not afraid of the dentist (OR 7.9 and p < 0.001) (Tab. IV).
Regarding patients with dental anxiety, there were significantly more patients (p = 0.003) who had a decrease in the STAI-YA score greater than 8 points in the VR group compared to the control group (respectively 75% and 37.5%) (Fig. 4) (Tab. V).
Side effects of VR and the desire or not to repeat the VR experience
No patient reported side effect such as headache, dizziness, or nausea, which would be like cybersickness.
96% of patients wanted to repeat the VR experience for futures surgeries.
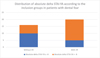 |
Fig. 4 Distribution of absolute delta STAI-YA according to the inclusion groups in patients with dental fear. p = 0.003; p = p-value; n (number of patients, 36); Absolute delta STAI-YA = Score STAI-YA(during) − Score STAI-YA(before); STAI-YA = State Trait Anxiety Inventory − State; VR = Virtual reality. |
Analyzes based on absolute delta STAI-YA.
Factors influencing STAI-YA score.
Results regarding patients with dental anxiety
Discussion
Virtual reality efficiency
This study demonstrated the effectiveness of virtual reality in reducing anxiety among adults undergoing dental extractions under local anesthesia.
Oral surgeons are faced with patient anxiety every day in surgeries performed under local anesthesia. The frequency of fear of the dentist is 20% in the UK and, among them, 10% are phobic [1,2]. It seems essential to improve the experience of patients and to seek solutions to reduce the anxiety because this one can lead to a vicious circle, as described by Armfield et al., in which patients wait until the last moment to consult. This delay in care sometimes leads to negative consequences on oral health with the presence of pain and therefore a bad experience during consultations with the surgeon [6].
Virtual reality is a non-drug method whose benefits on pain or anxiety have been reported in different health fields. In oral surgery, studies have mainly focused on the effectiveness of VR in reducing the pain or anxiety that children feel during dental care or surgery [15]. However, Hoffman et al. proved that adults were also receptive and that VR made it possible to reduce the pain felt during care for severe burn victims [9]. It was therefore legitimate to study the effectiveness of VR in a population of adults.
40% of patients who benefited from virtual reality had a decrease of the STAI-YA score of more than 8 points between before and during the intervention and the same percentage of patients was found concerning the reduction of the VAS anxiety by more than 2 cm (respectively p = 0.026 and p = 0.009 with a respective power of 85% and >90%). These significant results were in consistent with Yamashita's study, which found a reduced postoperative VAS of 1.33 cm ± 2.87 (p = 0.0014) in the VR group or studies of Mladenoviç et al. and Sweta et al. who observed a decrease in heart rate when adults wore the head-mounted display for dental avulsions [16–18]. Influencing factors of anxiety were found; patients who were afraid of the dentist in the VR group had a greater chance of reducing their anxiety during the procedure. In fact, 75% of adults with dental anxiety who were in the VR group decreased their STAI-YA anxiety score by more than 8 points. This confirms what Tanja-Dijkstra reported, the most anxious adults who benefit from virtual reality during dental procedures have the anxiety score that decreases the most [7]. In addition, 96% of adults in the VR group wished to repeat the experience. The same percentage were found in the studies of Yamashita et al. and Diaz-Orueta et al. [17,23].
Choice of questionnaires and scenarios
The STAI is the gold standard for the assessment of anxiety in clinical situations in psychiatry, medicine and surgery [20]. Spielberger created this scale in 1983 and he showed that the scale is sensitive to variations [19]. Beck showed that the Trait Scale (STAI-YB) correlated 0.73 with the Beck Depression Inventory and the State Scale (STAI-YA), the one used here, correlated 0.60 [24]. In the same way, Zemła et al. suggests psychological assessment of patients to identify or exclude depressed patients [20]. Without this, the risk is to obtain a less specific or falsely high result.
Here, patients followed by a psychiatrist for disorders such as depression were excluded and patients were asked about their daily consumption of anxiolytics, their addiction to tobacco or cannabis. Populations were comparable on the daily consumption of anxiolytics (p = 0.667), their addiction to tobacco (p = 0.706) or cannabis (p = 1). If there was an influence of these parameters, then it was present in an equivalent way in the two groups. Some limitations should be considered, such as the difficulty older people may have in completing the STAI-YA, the completion time (15 min) and the number of questions (20 items) [20]. Some elderly people were helped to complete the questionnaire, it may have influenced them.
The STAI-YA offers precise questions and the interpretation of the results is more standardized than that of the VAS which is patient dependent [20]. VAS is validated in the assessment of anxiety; it is said to be reliable, fast, and would be comparable to STAI-YA (21). VAS was not used as the main evaluation criterion but as a tool to confirm the choice of metric. The results was comparable regardless of the scale used, this reinforces results and the choice of STAI-YA as the primary endpoint was relevant.
A systematic review argues that the environment in which care take place influences the patient's well-being [25]. Exposure to a real or artificial nature reduces patient anxiety in a hospital waiting room compared to a usual neutral environment, with no significant difference between real or artificial flowers [26]. Diaz-Orueta et al. worked on a “Isla Calma” VR scenario with the goal of making it available to healthcare professionals to reduce patient stress. The nature landscapes with the presence of flowers, animals and the absence of humans were chosen because they are associated with a relaxing environment [23]. This explains the choice to work with Healthymind®, a company with doctors and engineers who work with a variety of natural landscapes. Here, regardless of the duration of the procedure, between ten minutes and one hour, no symptoms of cybersickness have been reported.
Study limitations
Lack of objective assessment
No per operative anxiety assessment was conducted in live, mainly to avoid the patient having to disengage from the immersive scenario. An endeavor was undertaken to transcribe anxiety with utmost accuracy by conducting interviews in close proximity to the intervention. It would have been appropriate to add an objective measurement in real time as with the evolution of the heart rate for example, like Yamashita et al. or Mladenoviç et al. [17,18].
Population
To determine the type of population, patients were questioned if they consider themselves to be afraid of the dentist. 32.0% reported being afraid of the dentist in the control group and 36.4% in the VR group. This is higher than the prevalence of the general population which is 20% [1]. Modified Dental Anxiety Scale (MDAS) has not been used because the multiplication of questionnaires could lose the interest of patients and lead to less reliable answers. Either the prevalence was overestimated due to a binary response, or the actual prevalence was higher, considering the study was conducted at a university hospital center where patients with higher anxiety levels, often excluded from dental clinics, were consulted.
In the VR group, the STAI-YA score was higher at baseline than in the control group. The population was also younger with an average age of 34.6 years compared to 43.7 years in the group without VR. Humphris et al. and Enkling et al. showed that young people, regardless of gender, were more anxious than older people [27,28]. The population of this study agrees with these studies. This difference in average age can be explained by the fact that some patients had to be changed group because the surgery was urgent, and the head-mounted virtual reality displays was not available at the time.
The study was open-label and randomized. Differences in mean age and baseline STAI-YA score between the two groups suggest that there were biases in randomization since the number of patients included was sufficient, so it was not a power problem (85%).
Perspectives
It would be interesting to use “active” virtual information, i.e., to give the patient the possibility of moving around in the virtual world in which he finds himself or even of playing a game using a joystick. The interactive side would make VR more sophisticated. Like Hoffman and al. shows, the more sophisticated VR is, the more effective it is [11]. Patients who have not been receptive to VR maybe need to have control over the situation, active VR would allow them to control the scene or the game using the joystick.
However, with an active VR the risk of cybersickness is increased. In the study by Furman and al., there is a significant difference in patients who had nausea with VR compared to film. VR was a landscape in which patients walked around using a joystick [29].
The interest of a third group with a black headset on the eyes to test the intrinsic efficiency of the software could be discussed.
Pain and anxiety are two interconnected elements, and it would have been relevant to assess the level of pain in patients.
The volume of the PICO G2® 3D helmet was problematic for the practitioner and the patient. The surgeon had always been able to adapt, but it was at the cost of uncomfortable postures for the back of the dental assistant and the practitioner. As for patients, some have complained of a blurred image caused by the practitioner's gestures moving the helmet.
Conclusion
Virtual reality seems effective in reducing the anxiety of adults who benefit for multiple dental avulsions under local anesthesia.
In the VR group, 40% of patients reduced their STAI-YA score by more than 8 points, which was significantly different than the 20% of the control group (p = 0.0026); the trend was the same with VAS. This outcome suggests the potential benefits of introducing virtual reality, particularly for adults who express fear or anxiety about dental visits. Indeed, 75% of adults with dental anxiety who were in the VR group decreased their STAI-YA anxiety score by more than 8 points.
No side effects were observed and a desire to repeat the virtual reality (VR) experience was expressed by 96% of the patients.
Funding
Thanks to the Healthymind company for the loan of head-mounted display PICO G2 3D and Bose headsets and for their involvement in proofreading the article. Thanks to Dr Morello Rémy (University Hospital of Caen) for producing the statistics, he was totally independent from the Healthymind company.
Conflicts of interest
None of the authors have any relevant financial relationship with a commercial interest.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, AP, upon reasonable request.
The data are not publicly available to avoid compromising the private information of the participants.
Author contribution statement
The writer was Anaïs Protin, resident in oral surgery and at the initiative of the study. The coordinating investigator was Dr. Alexis Veyssiere (department of maxillafacial surgery, Caen University Hospital); He revised it critically and approved the version to be published. Dr. Jean-François Sergent was a co-investigator in Caen University Hospital. Dorian Henry and Guillaume Gautier were also co-investigators from Caen University Hospital (residents in oral surgery). They participated in the recruitment of patients.
Informed consent
All patients signed a written consent after receiving oral and written explanations. They have benefited from the 7-day withdrawal period.
References
- Silveira ER, Cademartori MG, Schuch HS, Armfield JA, Demarco FF. Estimated prevalence of dental fear in adults: a systematic review and meta-analysis. J Dent 2021;108:103632. [CrossRef] [PubMed] [Google Scholar]
- Hill KB, Chadwick B, Freeman R, O'Sullivan I, Murray JJ. Adult Dental Health Survey 2009: relationships between dental attendance patterns, oral health behaviour and the current barriers to dental care. Br Dent J 2013;214:25‑32. [CrossRef] [PubMed] [Google Scholar]
- Oosterink FMD, De Jongh A, Aartman IHA. What are people afraid of during dental treatment? Anxiety-provoking capacity of 67 stimuli characteristic of the dental setting: anxiety-provoking stimuli in the dental setting. Eur J Oral Sci. 2008;116:44‑51. [CrossRef] [PubMed] [Google Scholar]
- Beaton L, Freeman R, Humphris G. Why are people afraid of the dentist? Observations and explanations. Med Princ Pract 2014;23:295‑ 301. [CrossRef] [PubMed] [Google Scholar]
- Yakar B, Kaygusuz TÖ, PiRiNçci E. Evaluation of dental anxiety and fear in patients who admitted to the faculty of dentistry: which patients are more risky in terms of dental anxiety. Ethiop J Health Sci 1970;29(6). Disponible sur: https://www.ajol.info/index.php/ejhs/article/view/191319 [CrossRef] [Google Scholar]
- Armfield JM, Stewart JF, Spencer AJ. The vicious cycle of dental fear: exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health. 2007;7:1. [CrossRef] [Google Scholar]
- Tanja-Dijkstra K, Pahl S, White M, Andrade J, Qian C, Bruce M, et al. Improving dental experiences by using virtual reality distraction: a simulation study. PLoS ONE 2014;9:e91276. [CrossRef] [PubMed] [Google Scholar]
- Rajeev A, Patthi B, Janakiram C, Singla A, Malhi R, Kumari M. Influence of the previous dental visit experience in seeking dental care among young adults. J Family Med Prim Care. 2020;9:609‑613. [CrossRef] [PubMed] [Google Scholar]
- Hoffman HG, Patterson DR, Carrougher GJ. Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: a controlled study. Clin J Pain 2000;16:244‑250. [CrossRef] [PubMed] [Google Scholar]
- Hoffman HG, Rodriguez RA, Gonzalez M, Bernardy M, Peña R, Beck W, et al. Immersive virtual reality as an adjunctive non-opioid analgesic for pre-dominantly Latin American children with large severe burn wounds during burn wound cleaning in the intensive care unit: a pilot study. Front Hum Neurosci. 2019;13:262. [CrossRef] [Google Scholar]
- Hoffman HG, Sharar SR, Coda B, Everett JJ, Ciol M, Richards T, et al. Manipulating presence influences the magnitude of virtual reality analgesia. Pain 2004;111:162‑168. [CrossRef] [PubMed] [Google Scholar]
- Ahmad M, Bani Mohammad E, Anshasi HA. Virtual reality technology for pain and anxiety management among patients with cancer: a systematic review. Pain Manag Nurs 2020;21:601‑607. [CrossRef] [PubMed] [Google Scholar]
- Gao J, Liu S, Zhang S, Wang Y, Liang Z, Feng Q, et al. Pilot study of a virtual reality educational intervention for radiotherapy patients prior to initiating treatment. J Canc Educ 2020. Disponible sur: https://link.springer.com/10.1007/s13187-020-01848-5 [Google Scholar]
- Ganry L, Hersant B, Sidahmed-Mezi M, Dhonneur G, Meningaud JP. Using virtual reality to control preoperative anxiety in ambulatory surgery patients: a pilot study in maxillofacial and plastic surgery. J Stomatol Oral Maxillofac Surg 2018;119:257‑261. [CrossRef] [PubMed] [Google Scholar]
- López-Valverde N, Muriel-Fernández J, López-Valverde A, Valero-Juan LF, Ramírez JM, Flores-Fraile J, et al. Use of virtual reality for the management of anxiety and pain in dental treatments: systematic review and meta-analysis. JCM 2020;9:3086. [CrossRef] [Google Scholar]
- Sweta V, Abhinav R, Ramesh A. Role of virtual reality in pain perception of patients following the administration of local anesthesia. Ann Maxillofac Surg 2019;9:110. [CrossRef] [PubMed] [Google Scholar]
- Yamashita Y, Shimohira D, Aijima R, Mori K, Danjo A. Clinical effect of virtual reality to relieve anxiety during impacted mandibular third molar extraction under local anesthesia. J Oral Maxillofacial Surg 2020;78:545.e1–545.e6. [CrossRef] [Google Scholar]
- Mladenovic R, Djordjevic F. Effectiveness of virtual reality as a distraction on anxiety and pain during impacted mandibular third molar surgery under local Anesthesia. J Stomatol Oral Maxillofac Surg 2021;122 (4): e15‑20. [CrossRef] [PubMed] [Google Scholar]
- Spielberger CD. State-trait anxiety inventory. In: Weiner IB, Craighead WE, éditeurs. The Corsini Encyclopedia of Psychology. Hoboken, NJ, USA: John Wiley & Sons, Inc; 2010 [cité 14 nov 2021]. p. corpsy0943. Disponible sur: https://onlinelibrary.wiley.com/doi/10.1002/9780470479216.corpsy0943 [Google Scholar]
- Zemła AJ, Nowicka-Sauer K, Jarmoszewicz K, Wera K, Batkiewicz S, Pietrzykowska M. Measures of preoperative anxiety. Anaesthesiol Intensive Ther. 2019;51:64‑69. [CrossRef] [PubMed] [Google Scholar]
- Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149‑158. [CrossRef] [PubMed] [Google Scholar]
- Galle C, Faivre T, Robin O. Evaluation comparative de l'anxiété induite par un acte chirurgical odontologique et dermatologique. Med Buccale Chir Buccale 2005;11:87‑96. [CrossRef] [EDP Sciences] [Google Scholar]
- Diaz-Orueta U, Alvarado S, Gutiérrez D, Climent G, Banterla F. “Isla Calma”, a novel virtual reality environment for pain and anxiety distraction: report on usability, acceptability, and subjective experience. Games Health J 2012;1:353‑361. [CrossRef] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consulting Clin Psychol 1988;56 (6): 893‑897. [CrossRef] [PubMed] [Google Scholar]
- Dijkstra K, Pieterse M, Pruyn A. Physical environmental stimuli that turn healthcare facilities into healing environments through psychologically mediated effects: systematic review. J Adv Nurs. 2006;56:166‑181. [CrossRef] [PubMed] [Google Scholar]
- Beukeboom CJ, Langeveld D, Tanja-Dijkstra K. Stress-reducing effects of real and artificial nature in a hospital waiting room. J Alternat Complement Med 2012;18:329‑33. [CrossRef] [PubMed] [Google Scholar]
- Humphris GM, Dyer TA, Robinson PG. The modified dental anxiety scale: UK general public population norms in 2008 with further psychometrics and effects of age. BMC Oral Health. 2009;9:20. [CrossRef] [Google Scholar]
- Enkling N, Marwinski G, Jöhren P. Dental anxiety in a representative sample of residents of a large German city. Clin Oral Invest. 2006;10:84‑91. [CrossRef] [PubMed] [Google Scholar]
- Furman E, Jasinevicius TR, Bissada NF, Victoroff KZ, Skillicorn R, B uchner M. Virtual reality distraction for pain control during periodontal scaling and root planing procedures. J Am Dent Assoc. 2009;140:1508‑16. [CrossRef] [Google Scholar]
All Tables
All Figures
 |
Fig. 1 Flow chart. |
| In the text | |
 |
Fig. 2 Distribution of groups according to absolute deltas. % = percentage of individuals concerned. Absolute delta STAI-YA = Score STAI-YA (during) − Score STAI-YA (before). Absolute delta VAS = Score VAS (during) − score VAS (before). STAI-YA = State Trait Anxiety Inventory − State VAS = Visual analogue scale (anxiety). VR = Virtual reality. |
| In the text | |
 |
Fig. 3 Power of the study as a function of sample size. |
| In the text | |
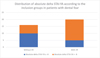 |
Fig. 4 Distribution of absolute delta STAI-YA according to the inclusion groups in patients with dental fear. p = 0.003; p = p-value; n (number of patients, 36); Absolute delta STAI-YA = Score STAI-YA(during) − Score STAI-YA(before); STAI-YA = State Trait Anxiety Inventory − State; VR = Virtual reality. |
| In the text | |
Current usage metrics show cumulative count of Article Views (full-text article views including HTML views, PDF and ePub downloads, according to the available data) and Abstracts Views on Vision4Press platform.
Data correspond to usage on the plateform after 2015. The current usage metrics is available 48-96 hours after online publication and is updated daily on week days.
Initial download of the metrics may take a while.


