| Issue |
J Oral Med Oral Surg
Volume 25, Number 3, 2019
|
|
|---|---|---|
| Article Number | 30 | |
| Number of page(s) | 4 | |
| Section | Cas clinique et revue de la littérature / Up-to date review and case report | |
| DOI | https://doi.org/10.1051/mbcb/2019021 | |
| Published online | 02 September 2019 | |
Up-to Date Review And Case Report
Lymphomatoid papulosis localized to the oral mucosa: case report and literature review
1
Service de chirurgie maxillo- faciale, chirurgie orale et odontologie hospitalière, Centre hospitalier Universitaire et régional de Besançon, Besançon, France
2
Service de chirurgie maxillo- faciale, stomatologie et chirurgie orale, Centre hospitalier Lyon-Sud, Hospices Civils de Lyon, Pierre-Bénite, France
3
Faculté d'odontologie et Centre Léon Bérard, Lyon, France
* Correspondence: bretsophie@gmail.com
Received:
6
February
2019
Accepted:
9
July
2019
Introduction: Lymphomatoid papulosis is a primary CD 30+ cutaneous lymphoproliferation. Observation: We report the case of a 39-year-old patient who presented with ulcers on the back of the tongue, gums, buccal mucosa, and soft palate, which evolved as spontaneously regressive flare-ups. The diagnosis of inflammatory bowel disease was initially proposed. Several years later, the patient presented an ulcer on the left middle finger. Histological examination confirmed the diagnosis of lymphomatoid papulosis. Discussion: This chronic dermatosis manifests a single rash or multiple papulonodular rashes, evolving as spontaneously regressive flare-ups. Mucosal involvement is rare, and no prognostic factor for this location has been highlighted to this date. Pathological examination is essential. Conclusion: The mucosal involvement of lymphomatoid papulosis is one of the diagnoses to be considered for recurrent mouth ulcers.
Key words: oral lymphomatoid papulosis / diagnosis / oral mucosal disease
© The authors, 2019
 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
According to the World Health Organization-European Organization for Research and Treatment of Cancer (WHO-EORTC) classification [1], lymphomatoid papulosis (LP) belongs to the group of primary cutaneous CD30+ lymphoproliferations with good prognosis similar to the cutaneous lymphoma with large anaplastic cells. It is characterized by a chronic papulo-nodular rash, evolving as spontaneously regressive flare-ups. Mucosal involvement is rare, with 22 cases having been described in the literature, in all of which mucous membranes combined [2].
Observation
We report the case of a 39-year-old woman who visited the dermatology department of Centre Hospitalo- universitaire for the first time in October 2013 for a large painful ulceration ∼2 cm in diameter with infiltrated edges on the right edge of the tongue that appeared a week before.
This patient presented a history of gastroplasty and herpes labialis with an episode of erythema nodosum as well as an area of allergic response.
The general condition was preserved. Initial diagnosis of herpetic recurrence was made, and an antiviral treatment was prescribed, without any clinical improvement. The lesion then disappeared spontaneously in 15 days. In September 2014, the patient was re-examined in emergency service for ulcerations affecting the right dorso-lateral part of the tongue and the soft palate (Figs. 1 and 2).
Allergic etiology was initially considered, and dermocorticoids and antiallergics were prescribed.
In October 2015, ulcerated lesions appeared on the hands, palms, and fingertips. Mucosal lesions continued to evolve as spontaneously regressive flare-ups in approximately 15 days, leaving a small scar that disappeared in a week. The mucosa remained healthy for 4–6 weeks. Chronic inflammatory bowel disease was suspected.
In September 2017, a biopsy of a hand lesion established the diagnosis of LP type A. In February 2018, histopathological and immunohistochemical analyses of a tongue lesion showed a lymphocytic infiltrate with large CD30 + cells, confirming the mucosal involvement of this pathology (Figs. 3–5).
The patient later reported lesions on the eyelids, nostrils, and scalp, leaving unsightly scars that were hard to live with.
For the expressed discomfort, treatment with oral methotrexate 7.5 mg per week was initiated. A 6-week follow-up consultation after the start of treatment showed improvement in flare-up intensity. Regular consultations with the dermatologist every 3 months have shown an improvement in the frequency of flare-ups.
 |
Fig. 1 Intraoral photograph. Ulcerations with infiltrated edges on the dorso-lateral right side of the tongue. |
 |
Fig. 2 Intraoral photograph. Ulcerations of the left palatal veil. |
 |
Fig. 3 Histopathological examination of the biopsy (standard magnification ×10; Hematoxylin–Phloxine–Saffron (HPS) stain). Upper arrow: ulceration; Bottom arrow: infiltrate within the predominantly mononuclear chorion. |
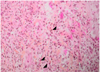 |
Fig. 4 Histopathological examination of the lesion (standard magnification ×40; HPS stain). |
 |
Fig. 5 Immumohistochemical analysis of the biopsy (standard magnification ×10). Staining of multiple CD30 cells. |
Discussion
LP is a benign CD 30+ cutaneous lymphoproliferation. First described by Macaulay in 1968 as a chronic, papulonodular or papulonecrotic, recurrent, autoregressive rash with histological abnormalities of malignant appearance, LP can affect the entire skin surface, with the most common sites being upper body and limbs [3].
Sioutos et al. reported the first case of oral manifestation of LP in 1997. They described the case of a 60-year-old man who presented with a lesion on the tongue as the first manifestation of LP [4].
Since then, 21 cases of oral mucosa LP have been reported [2,5–13] (Tab. I). Most often, lesions are nodular, with infiltrated edges, erythematous, fibrinous, ulcerated, and painful. They evolve as spontaneously regressive flare-ups in 2–8 weeks, sometimes leaving small scars. The general condition of the patients' is preserved. The most frequent affected areas are the tongue and lip mucosa, although the lesions can appear across the entire oral mucosa. The injuries of the palatal veil have never been described until now. LP affects women more frequently than men (8 men to 15 women), and the age of diagnosis ranges from 33 to 83 years.
In majority of the cases, the mucosal lesions appear before the cutaneous lesions (14/22; 1 case without cutaneous manifestation of LP).
Fewer than 20% of the cases of LP are associated with a lymphoid malignancy previously developed during or after lymphomatoid papulosis. To date, no prognostic factors for this unfavorable development have been demonstrated [14]. Several histological types of LP have been described according to their immunohistochemical aspects, without any prognostic value [15]. Type A LP is characterized by a mixed triangular lymphocyte infiltrate containing large CD30+ tumor cells and inflammatory cells. Type B LP presents a CD30+ T lymphocyte epidermotropic infiltrate. Type C LP presents large atypical a CD30+ cells layer. Type D LP presents CD30+ and CD8+ lymphocytes with a TIA-1 cytotoxic mark. Type E LP presents an angiocentric and angiodestructive infiltrate with CD30+ T lymphocytes. LP type A is the most frequently encountered histological form [16]. Mucosal involvement is not associated with a particular type and does not influence the prognosis [17].
Therapeutic restrain is recommended in the case of a localized and minimally debilitating LP. Treatment with low-dose methotrexate (5–30 mg/week orally or by injection) or phototherapy (psoralen and ultraviolet A [PUVA] therapy) can be recommended to patients with multiple lesions, disseminated or esthetically debilitating [16]. These two treatments reduce the number of lesions during LP flare-ups as well as accelerate lesion regression.
However, upon treatment discontinuation or dose reduction, approximately 40% of the patients relapse. Thus, it is necessary to continue the initiated treatment for a long-term while monitoring potential side effects (hepatic fibrosis for methotrexate and skin cancers for PUVA therapy).
In patients requiring treatment, the possible side effects, long-term complications, and costs of the suggested treatment must be weighed against the prognosis of the LP.
In conclusion, the mucosal involvement of LP is rare. Thus, it is important to recognize this particular clinical presentation to avoid diagnostic and therapeutic errors.
Cases of lymphomatoid papulosis identified in the literature.
Conflicts of interests
The authors declare that they have no conflicts of interest in relation to the publication of this article.
References
- Willemze R. WHO-EORTC classification for cutaneous lymphomas. Blood 2005;105:3768–3785. [CrossRef] [Google Scholar]
- Schwartz Z, Coleman M, Toyohara JP, Freedman PD, Magro CM. Oral lymphomatoid papulosis type C: a diagnostic pitfall, often confused with T-cell lymphoma. Ann Diagnos Pathol 2017;31:50–55. [CrossRef] [Google Scholar]
- Macaulay WL. Lymphomatoid papulosis. A continuing self-healing eruption, clinically benign-histologically malignant. Arch Dermatol 1968;97:23–30. [CrossRef] [PubMed] [Google Scholar]
- Sioutos N, Asvesti C, Sivridis E, Aygerinou G, Tsega A, Zakopoulou N, et al. Lymphomatoid papulosis type A: clinical, morphologic, and immunophenotypic study. Int J Dermatol 1997;36:514–517. [CrossRef] [PubMed] [Google Scholar]
- Kato N, Tomita Y, Yoshida K, Hisai H. Involvement of the tongue by lymphomatoid papulosis. Am J Dermatopathol 1998;20:522–526. [CrossRef] [PubMed] [Google Scholar]
- Sciubba J, Said-al-Naief N, Fantasia J. Critical review of lymphomatoid papulosis of the oral cavity with case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont 2000;90:195–204. [CrossRef] [Google Scholar]
- Chimenti S, Fargnoli MC, Pacifico A, Peris K. Mucosal involvement in a patient with lymphomatoid papulosis. J Am Acad Dermatol 2001;44(2 Suppl):339–341. [CrossRef] [PubMed] [Google Scholar]
- Serra-Guillén C, Requena C, Alfaro A, Hueso L, Sanmartín O, Llombart B, et al. [Oral involvement in lymphomatoid papulosis]. Actas Dermosifiliogr 2007;98:265–267. [CrossRef] [PubMed] [Google Scholar]
- Pujol RM, Muret MPG, Bergua P, Bordes R, Alomar A. Oral involvement in lymphomatoid papulosis. Dermatology 2005;210: 53–57. [CrossRef] [PubMed] [Google Scholar]
- Allabert C, Estève E, Joly P, Troussard X, Comoz F, Courville P, et al. Atteinte muqueuse dans la papulose lymphomatoïde: quatre cas. Ann Dermatol Vénéréolog 2008;135:273–278. [CrossRef] [Google Scholar]
- Agarwal M, Shenjere P, Blewitt RW, Hall G, Sloan P, Pigadas N, et al. CD30-Positive T-Cell Lymphoproliferative Disorder of the Oral Mucosa—An Indolent Lesion: Report of 4 Cases. Int J Surg Pathol 2008;16:286–290. [CrossRef] [PubMed] [Google Scholar]
- de-Misa RF, García M, Dorta S, Febles C, Hernández-Machín B, Serrano S, et al. Solitary oral ulceration as the first appearance of lymphomatoid papulosis: a diagnostic challenge. Clin Experiment Dermatol 2010;35:165–168. [CrossRef] [Google Scholar]
- Booken N, Heck M, Peitsch W, Goerdt S, Klemke C. Ulcerated nodules on the oral mucosa and fingers: a quiz. Acta Dermato Venereolog 2013;93:250–252. [CrossRef] [Google Scholar]
- Bekkenk MW, Geelen FAMJ, van Voorst Vader PC, Heule F, Geerts M-L, van Vloten WA, et al. Primary and secondary cutaneous CD30+lymphoproliferative disorders: a report from the Dutch Cutaneous Lymphoma Group on the long-term follow-up data of 219 patients and guidelines for diagnosis and treatment. Blood 2000;95:3653–3661. [Google Scholar]
- de Souza A, el-Azhary RA, Camilleri MJ, Wada DA, Appert DL, Gibson LE. In search of prognostic indicators for lymphomatoid papulosis: A retrospective study of 123 patients. J Am Acad Dermatol 2012;66:928–937. [CrossRef] [PubMed] [Google Scholar]
- Kempf W, Pfaltz K, Vermeer MH, Cozzio A, Ortiz-Romero PL, Bagot M, et al. EORTC, ISCL, and USCLC consensus recommendations for the treatment of primary cutaneous CD30-positive lymphoproliferative disorders: lymphomatoid papulosis and primary cutaneous anaplastic large-cell lymphoma. Blood 2011;118: 4024–4035. [CrossRef] [Google Scholar]
- Benslama L, Andre CV, Charlotte F, Agbo-Godeau S, Goudot P. Papulose lymphomatoïde de localisation muqueuse: deux cas. Rev Stomatolog Chirurg Maxillo-faciale Chirurg Orale 2015;116: 111–113. [CrossRef] [Google Scholar]
All Tables
All Figures
 |
Fig. 1 Intraoral photograph. Ulcerations with infiltrated edges on the dorso-lateral right side of the tongue. |
| In the text | |
 |
Fig. 2 Intraoral photograph. Ulcerations of the left palatal veil. |
| In the text | |
 |
Fig. 3 Histopathological examination of the biopsy (standard magnification ×10; Hematoxylin–Phloxine–Saffron (HPS) stain). Upper arrow: ulceration; Bottom arrow: infiltrate within the predominantly mononuclear chorion. |
| In the text | |
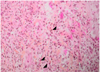 |
Fig. 4 Histopathological examination of the lesion (standard magnification ×40; HPS stain). |
| In the text | |
 |
Fig. 5 Immumohistochemical analysis of the biopsy (standard magnification ×10). Staining of multiple CD30 cells. |
| In the text | |
Current usage metrics show cumulative count of Article Views (full-text article views including HTML views, PDF and ePub downloads, according to the available data) and Abstracts Views on Vision4Press platform.
Data correspond to usage on the plateform after 2015. The current usage metrics is available 48-96 hours after online publication and is updated daily on week days.
Initial download of the metrics may take a while.


