| Issue |
J Oral Med Oral Surg
Volume 25, Number 2, 2019
|
|
|---|---|---|
| Article Number | 20 | |
| Number of page(s) | 3 | |
| Section | Cas clinique / Short case report | |
| DOI | https://doi.org/10.1051/mbcb/2019004 | |
| Published online | 26 April 2019 | |
Short Case Report
From dental infection to extradural empyema: a case report
Service d'Odontologie, CHU Nancy, Nancy, France
* Correspondence: clemcomte@gmail.com
Received:
23
October
2018
Accepted:
11
March
2019
Introduction: Brain infections of dental origin are rare, but well-known and accurately described. There are two different brain infections: brain abscess, the most frequent, and extradural or subdural empyema. Here, we discuss the case of an extradural empyema. Observation: A 28-year-old man with a very poor dental condition showed neurological and eye infection signs. A brain and face CT scan revealed extradural empyema, orbit abscess and pansinusitis. These infections had all dental origin: an apical lesion of tooth 26. Discussion: Such severe cases must be surgically and medically treated with a strong antibiotic therapy. A systematic investigation and the treatment of dental infected areas are both necessary.
Key words: empyema / extradural / dental / brain /
© The authors, 2019
 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Observation
A 28-year-old man weighing 125 kg with no prior history of medical or surgical treatments was urgently addressed. The physical examination showed left exophthalmos, eyelid edema and diplopia. A pulsatile left-sided frontal headache increased by anteflexion and a painful face swelling were also reported. Symptoms started 4 days before, after regular intakes of nonsteroidal anti-inflammatory drugs (NSAIDs). Sweating and shivering were also experienced by the patient in the previous 3 days. The patient did not show any signs of rhinorrhea, difficulty in swallowing, breathing disorders or heart disorders. Lab test results revealed an inflammatory syndrome with a C-reactive protein concentration of 220 mg/L.
The urgently performed face CT scan detected left-sided maxillary sinusitis, ethmoiditis, intraorbital abscess, frontal sinusitis and a brain empyema of 15 × 16 mm (Figs. 1–3).
An urgent medico-surgical treatment was conducted to eviscerate and abundantly irrigate the left frontal maxillary sinus. It included left meatotomy and recanalized of the frontal sinus. A drainage by left canthotomy was performed to treat the intraorbital subperiosteal abscess.
The evidence-based infection notice led to implement a triple antibiotic therapy consisting of 12 g/day of Cefotaxime + 12 g/day of Fosfomycin and 1500 mg/day of Metronidazole.
Then, the patient was transferred to the Neurosurgery Department of the academic-based hospital of Nancy.
An oral surgery visit revealed several dental infection areas, in particular an apical lesion on teeth 18, 16 and 26 (Fig. 4). A surgical operation was carried out to remove all the dental infection areas. Unfortunately, the patient's condition worsened and needed a neuro-surgical operation: 3 weeks after the first operation, a craniotomy was performed to drain and irrigate the extradural empyema.
The blood cultures were positive to the Streptococcus anginosus, a bacterium found in the mucous membrane, making part of the ENT area. This proved that the infection had a dental origin. The antibiotic therapy was adjusted after the results and maintained for 8 weeks. 3 g Cefotaxime was administered 4 times a day, and 600 mg Rifampicin twice a day.
The patient was sent back home 1 month and a half after the beginning of the care process.
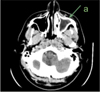 |
Fig. 1 Left maxillary sinusitis of dental origin. |
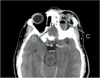 |
Fig. 2 Ethmoiditis and intraorbital abscess. |
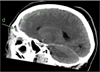 |
Fig. 3 Frontal sinusitis and extradural empyema. |
 |
Fig. 4 Apical cyst of tooth 26. |
Discussion
Brain infections of dental origin are well-known and accurately described [1,2]. The most frequently found are abscesses due to blood contamination. Empyemas result from an infection transmitted to adjacent cavities due to otitis, frontal sinusitis or a post-surgical or post-traumatic direct inoculation [3]. A brain abscess is a pus collection in the brain parenchyma, while an intracranial empyema is a pus collection in the subdural or extradural area. The incidence is low (1 per 100 000 population per year). The prevalence is higher in children and young adults, and male subjects are 1.5–3 times more likely to be affected [3].
Despite medical imaging making the diagnosis faster and the introduction of antibiotic therapies, the mortality rate for empyema, in particular for subdural empyema, is still high: about 10%. The morbidity rate is 8–21% [4]. Some consequences are frequently observed: up to 33% neurological disorder and 15% epilepsy cases are reported [5].
Here, we discuss a case of extradural empyema. The origin of brain empyemas is mainly the sinus: a bacterial propagation among adjacent cavities can be easily tracked. Here, the dental infection area (teeth 26) contaminates the maxillary sinus, then the ethmoid sinus; then, the orbital and the frontal sinus are affected and the infection reaches the extradural area. The symptoms become more eloquent. The infection and the compression on the eyeball and the brain must be urgently treated.
The clinical signs related to this condition must be known to be early detected.
The signs of both empyema and brain abscess are headache, fever, neurological disorder, disturbance of consciousness and focal neurological deficits. A generalized tonic–clonic seizure may also facilitate diagnosis. Exophthalmos, ophthalmoplegia and visual impairment linked or not to an inflammatory syndrome are observed in intraorbital abscess. Signs of pansinusitis and dental infection may also be detected.
A 1st-line brain CT scan must be performed to establish the diagnosis. Empyemas appear as extracerebral crescent-shaped (for subdural empyema) or convex (for extradural empyema) hypodense areas with peripheral contrast enhancement. Lab test results reveal an inflammatory syndrome in 70% of cases. Blood culture must be performed as soon as possible.
Treatments are not standardized. Every condition requires a specific urgent, multidisciplinary and medico-surgical management based on a long-term antibiotic therapy lasting 6–8 weeks. A high dosage of 3rd-generation cephalosporin is usually administered in association with imidazole before the antibiotic susceptibility testing is done. To avoid intracranial hypertension, Mannitol may be prescribed in association with an anti-epileptic and an anticoagulant treatment if a risk of cerebral thrombophlebitis is found. All infectious areas, namely those found on teeth, must be detected and treated. A constant monitoring must also be carried out until normalization is achieved.
The S. milleri group makes part of the oropharyngeal flora bacteria and consists of three species: S. anginosus, S. intermedius and S. constellatus [5]. If the infection is of sinus origin, this group is the most frequently found (18%), followed by staphylococci (17%) and Gram-negative bacteria (15%). S. pneumoniae is found if the origin of the infection is otological.
Taking NSAIDs is a likely risk factor, or at least an aggravating factor, even though no studies could scientifically prove it [6]. NSAIDs alleviate symptoms and delay diagnosis. They reduce the synthesis of prostaglandins and impair polynuclear cells' functioning (adhesion, aggregation, chemotaxis and phagocytosis), jeopardizing the antibacterial activity. The NSAIDs' over-the-counter availability and their prescription to treat infections is a key issue.
Conclusion
An extradural empyema is a very serious condition with high morbidity and mortality. The life-threatening contamination from a dental infected area in a young patient with no prior medical history proves that any physicians must be aware of it to act properly. A systematic investigation and the treatment of dental infected areas are both necessary.
References
- Boisrame-Gastrin S, Legens M, Predine-Hug F. Abcès cérébraux d'origine dentaire, une porte d'entrée à ne pas méconnaître: à propos d'un cas. Méd Buccale Chir Buccale 2005;11: 175–180. [CrossRef] [Google Scholar]
- Page C, Lehmann P, Jeanjean P, Strunski V, Legars D. Abcès et empyèmes intracrâniens d'origine O.R.L. Ann Fr Oto-Rhino-Laryngol Pathol Cervicofac 2005;122:120–126. [Google Scholar]
- Bartt RE. Cranial epidural abscess and subdural empyema. Handb Clin Neurol 2010;96:75–89. [Google Scholar]
- Emery E, Redondo A, Berthelot JL, Bouali I, Ouahes O, Rey A. Abcès et empyèmes intracrâniens: prise en charge neurochirurgicale. Ann Fr Anesth Réanim 1999;18:567–573. [CrossRef] [Google Scholar]
- Patel AP, Masterson L, Deutsch CJ, Scoffings DJ, Fish BM. Management and outcomes in children with sinogenic intracranial abscesses. Int J Pediatr Otorhinolaryngol 2015;79:868–873. [CrossRef] [PubMed] [Google Scholar]
- Bennani-Baïti AA, Benbouzid A, Essakalli-Hossyni L Cervicofacial cellulitis: the impact of non-steroidal anti-inflammatory drugs. A study of 70 cases. Eur Ann Otorhinolaryngol Head Neck Dis 2015;132:181–184. [CrossRef] [PubMed] [Google Scholar]
All Figures
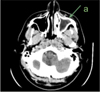 |
Fig. 1 Left maxillary sinusitis of dental origin. |
| In the text | |
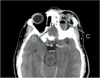 |
Fig. 2 Ethmoiditis and intraorbital abscess. |
| In the text | |
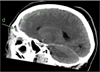 |
Fig. 3 Frontal sinusitis and extradural empyema. |
| In the text | |
 |
Fig. 4 Apical cyst of tooth 26. |
| In the text | |
Current usage metrics show cumulative count of Article Views (full-text article views including HTML views, PDF and ePub downloads, according to the available data) and Abstracts Views on Vision4Press platform.
Data correspond to usage on the plateform after 2015. The current usage metrics is available 48-96 hours after online publication and is updated daily on week days.
Initial download of the metrics may take a while.


