| Issue |
J Oral Med Oral Surg
Volume 29, Number 4, 2023
|
|
|---|---|---|
| Article Number | 38 | |
| Number of page(s) | 5 | |
| DOI | https://doi.org/10.1051/mbcb/2023044 | |
| Published online | 22 January 2024 | |
Original Research Article
Salivary cortisol and alpha amylase enzyme levels in different phases of minor recurrent aphthous stomatitis
1
Department of Oral Diagnostic Sciences, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia
2
Department of Medical Microbiology and Parasitology, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia
* Correspondence: gmansour@kau.edu.sa
Received:
24
August
2023
Accepted:
6
December
2023
Objectives: Recurrent aphthous stomatitis (RAS) is one of the most common oral mucosal lesions and stress is one of the major factors implicated in its causation. The aim of the present work is to measure the stress biomarkers, salivary cortisol (SC) and salivary alpha amylase (SAA), in the different phases of RAS. Patients and Methods: The study included 69 subjects of whom 38 patients served as the study group who suffered from minor RAS and one to three active minor oral ulcers of <48 h duration. The remaining 31 healthy subjects served as controls. Unstimulated salivary samples were collected twice from the study group; during the ulcerative phase of RAS and after complete healing has occurred, and only once from the controls. Concentrations of SC, and SAA enzyme were assessed by Enzyme-linked Immunosorbent Assay (ELISA). Results: There was a significant increase of SC and SAA in both the ulcerative and the post-healing phases in comparison to the control group. The ulcerative phase had higher but insignificant levels of both biomarkers when compared to the post-healing phase. There was a significant correlation between both biomarkers in the post-healing but not in the ulcerative phase. Conclusion: RAS patients have significantly higher levels of both stress biomarkers (SC and SAA) in the ulcerative and in the post-healing phases when compared to controls.
Key words: Recurrent aphthous stomatitis / salivary alpha-amylase / cortisol
© The authors, 2023
 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
RAS is among the most common oral mucosal lesions in the population worldwide, with a frequency of 5% to 50% [1,2]. RAS is characterized by recurring ulcers confined to the oral mucosa in otherwise healthy patients. The onset of RAS usually begins in adolescence, is most common in individuals in their 20s, and its frequency decreases with age. It negatively affects the quality of life, and may severely interfere with eating, speaking, and swallowing. Based on the size, number, and duration of the ulcer, RAS is classified into four specific classes: minor, major, severe and herpetiform [1].
Minor RAS is the most common form, affecting 70% to 87% of the population with RAS. Minor aphthae are generally located on lining mucosa: labial or buccal mucosa, the soft palate, and the floor of the mouth. They are shallow and may be single or multiple. Patients with minor RAS usually have 1 to 5 ulcers at each episode, with each lesion less than 1 cm in diameter. These ulcers are self-limiting and can resolve in 4 to 14 days, with an average of 10 days, without scarring [2].
A plethora of causative factors have been linked to the occurrence of RAS, including genetic tendency, hypersensitivity, immunological, nutritional, and microbial variables [3]. Moreover, RAS has been proposed to be associated with stress and anxiety, which impact the immune system components [4].
Anxiety and stress can be risk factors for oral lesions including RAS. Oral diseases can be affected by emotional or psychological changes directly or indirectly. Psychological factors can change nervous system markers (catecholamines, adrenaline, noradrenaline, and dopamine), hormonal system markers (cortisol, aldosterone), and immune system (T cells, B cells, natural killer cells, and immunoglobulins) causing initiation and progression of some oral diseases including RAS [5].
It is well known that stress may induce the release of cortisol which is a hormone produced in the adrenal cortex in response to stress through the hypothalamus − pituitary −adrenal (HPA) axis. The production of cortisol by the adrenal cortex is initiated by the production of corticotropin −releasing hormone (CRH) in the hypothalamus, which in turn, activates the secretion of adrenocorticotrophic hormone (ACTH) from the pituitary gland. The ACTH stimulates the adrenal cortex to secrete glucocorticoids (cortisol) [6].
SC measurement is considered to be an excellent indicator of plasma free cortisol concentration, escaping the biological changes due to corticosteroid binding globulin alterations and providing a feasible approach to assess pituitary adrenal function [7]. SC has been used in several studies as a marker of stress in RAS; however, the results of these studies are inconsistent [7–9].
SAA enzyme is the most distinguished of salivary enzymes. It breaks starch into maltose. The secretion of SAA is controlled by sympathetic autonomic nervous system (ANS) activity which significantly manages the stress psychobiology. Increased levels of SAA have been demonstrated in humans with physical and psychological stress. For this reason, the SAA has become a marker of stress and anxiety, being a fast, painless, and noninvasive tool for assessment of the ANS pathological dysregulation in specific clinical and subclinical conditions [10].
There is a potential role for noninvasive, real-time, and point-of-care biomarkers such as SC and SAA to identify the role of stress in etiopathogenesis of RAS. As both enzymes act as biological biomarkers of stress, an association, if possible, of their levels during RAS lesions would suggest a causal effect of stress on the occurrence of RAS. In previous studies, SC and SAA were compared between patients and controls [9,10]. However, very scarce literature was found comparing SC and SAA levels in ulcerative and healing phases of RAS.
The controversies in the association of stress biomarkers in RAS in different studies and the rarity of papers addressing the levels of these biomarkers in the different phases of RAS have been the stimulus for conducting the present study.
Materials and methods
The aim of the present study was to assess SC and SAA levels in relation to different phases of minor RAS and to compare them to normal controls.
The present study was approved by the research ethics committee. An informed consent was obtained from all the patients. The study was conducted in a university dental hospital on 69 subjects of whom 38 were the RAS group and 31 were age, sex, and socioeconomic status matched controls. The RAS group consisted of 21 males and 17 females. They presented with a history of minor RAS and one to three active minor oral ulcers of <48 h duration. The control group consisted of 16 males and 15 females. For their inclusion as controls, volunteers should never have presented oral ulcers, and except for the absence of lesions, this group shared the same inclusion and exclusion criteria with the RAS group.
Exclusion criteria included ulceration as a manifestation of a systemic disease, smoking, pregnancy, lactation, dental surgery within two weeks of study entry, local irritating factors that could lead to lesions as sharp cusps, improper fillings, or orthodontic appliances, or if participants suffered from immune deficiency, systemic, metabolic, or endocrine disease. Subjects receiving concomitant medications that could interfere with study evaluation were excluded from participation.
Unstimulated salivary samples were collected twice from the study group; during the ulcerative phase of RAS and after complete healing has occurred. Salivary samples were collected only once from the control group. All samples were taken during the morning period (8-10 am) to minimize the effect of the diurnal variation of salivary proteins or circadian rhythm. All participants were required not to eat, drink, or do oral hygiene measures nor put any substance in the mouth (including brushing teeth), do physical exercises, or use drugs or cosmetics in lips for at least 1 h before the sample collection to decrease its impurities. Prior to collection of salivary samples, they rinsed the mouth with water only without using any substance to enhance salivary secretion, and then spit saliva in a special sampling container. The samples were refrigerated at (4°C) awaiting analysis within 14 days. Concentrations of SC, and SAA enzyme were assessed by ELISA, according to manufacturer's instructions.
Statistical analysis
The gathered data were analyzed by the SPSS software (version. 22, IBM, Chicago, Illinois, USA). The paired t-test was used in the RAS group, to compare SC and SAA levels between ulcerative and healing RAS phases. SC level and SAA levels were compared between RAS and control groups by unpaired t-test. To assess the correlation between SC and SAA levels, the Pearson correlation coefficient was calculated. The significance level was set at 0.05.
Results
The age of the control group ranged from 18 to 31 yr with a mean of 24.8 yr, whereas the age of RAS group ranged from 18 to 33 yr with a mean of 25.3 yr.
The means and standard deviation of the SC and SAA in the control and RAS groups are shown in Table I.
There was a significant increase of SC in both the ulcerative and the post-healing phases in comparison to the control group. (p = 0.0001 and 0.004 respectively). In the RAS group, the ulcerative phase had a higher SC than the post-healing phase, but the results were not significant (p = 0.88) (Tab. I).
There was also a significant increase of SAA in both the ulcerative and the post-healing phases in comparison to the control group. (p = 0.0001 and 0.047 respectively). In the RAS group, the ulcerative phase had a higher SAA than the post-healing phase, but the results were not significant (p = 0.054) (Tab. I).
There was a strong positive correlation between levels of SC and SAA in the post-healing phase, (r = 0.685, and p-value = < 0.01). On the other hand, this correlation was insignificant in the ulcerative phase (Figs. 1 and 2).
Comparison of salivary Alpha amylase and salivary cortisol between control group and RAS patients during the ulcerative and post-healing phases.
 |
Fig. 1 Graph showing correlation between SAA and SC in the ulcerative phase. |
 |
Fig. 2 Graph showing correlation between SAA and SC in the post-healing phase. |
Discussion
RAS is believed to be a stress-related reaction. Several studies have found a positive correlation between stress as well as anxiety and RAS [4,11–14]. Stress was found to be the main predisposing factor for recurrent oral ulcers in previous investigations [4,15]. Stressful incidences may initiate fresh RAS episodes, particularly in patients with a history of RAS [15]. However, other researchers failed to find a link between stress and recurrent oral ulcers [16].
Psychosocial stress induces adaptational responses of physiologic systems with increasing activities in the HPA as well as in the ANS system. Cortisol levels reflect the HPA activity, whereas SAA represents the ANS activity [6,10]. It could be assumed that even a slight rise of SAA enzyme alongside dysregulation in the defensive immune components could trigger the occasion of RAS. In addition, supported ascent in cortisol levels with amylase could induce the pathophysiological events for ulcer proceeding [9].
While it is believed that psychological disorders may play a role in development of RAS, it was also argued that the elevated SC in RAS might be due to pain associated with oral ulcers inducing stress [17]. This also applies to SAA where Shirasaki et al. [18] found a significant correlation with pain severity and SAA (p < .01) and suggested it as a good index for measuring pain intensity.
Being a simple and noninvasive procedure, collection of salivary samples has increasingly gained popularity as a diagnostic marker for many diseases, in the field of oral cancer, Sjögren syndrome, diabetes [19], as well as in stress research [20]. In addition, SC may give a superior assessment of stress reaction in comparison to serum cortisol because it estimates the unbound cortisol level more precisely [21].
As SC and SAA are established biomarkers of both the HPA and ANS activities respectively, it seems more comprehensive to study both, in order to elucidate the role of stress in the etiology of RAS. Being an objective measure, salivary biomarkers are more representative of stress than self-administered questionnaires which often show inconsistent results [22]. A recent study found a positive correlation of both biomarkers in RAS. However, little has been mentioned about the level of these biomarkers in the different phases of RAS [23].
The association of stress and RAS has therapeutic implications on the treatment of RAS and stress management might be beneficial in those patients.
In the current work, significant increases in the levels of SC and SAA were found in RAS patients, compared to the control group, adding to the evidence that there is a relationship between RAS and stress biomarkers, and denoting a potential role of stress in development of RAS.
Our results of increased SC in RAS patients are in accordance with the findings previously revealed by Nadendla et al. [8], McCartan et al. [13], Albanidou-Farmaki et al. [14], Zakaria and Hosny [23], and Nurdiana et al. [24] suggesting that stress might have an important role in the aetiology of RAS.
On the other hand, dissimilar findings were reported by Kunikullaya et al. [9] who showed no significant difference in SC between RAS group and controls, and Vandana et al. [25] who reported no relation between SC and RAS.
In the present work, we found a significant increase of SC in the post-healing phase of RAS when compared to controls. Similar findings were obtained by Nadendla et al. [8] and Susanto et al. [17]. Moreover, the findings of the present study revealed increase in SC in the ulcerative phase in comparison to the post-healing phase. On the contrary, Rezaei et al. [7] reported decreased SC level in RAS group when compared to controls, as well as a non-significant difference between ulcerative and healing RAS phases. Cortisol secretion is controlled by the HPA axis, and it changes in relation to acute and chronic stress. In case of stress, the increase in the level of cortisol is preserved and it is straight forwardly corresponding to the seriousness of stress. Stress and anxiety hasten the event of RAS with rises in SC levels [4,13]. Therefore, the high level of SC in the post-healing RAS phase might be explained by a concomitant chronic anxiety and stress in these patients. Another explanation was proposed by Susanto et al. [17] who found a significantly high SC in untreated oral ulceration in patients with healed RAS compared to those who received local steroids. They assumed that untreated oral ulcers may have more inflammation which induces stress in RAS patients.
Since some authors have suggested the association of psychological disorders with RAS and considering that SAA is a marker of sympathetic ANS activation, the current study evaluated the enzyme level in different phases of RAS and revealed elevated levels in RAS patients when compared to controls. Similarly, a recent study reported significantly high difference in the mean of SAA levels between the patients having RAS and the control group [23]. On the contrary, Kunikullaya et al. [9] and Cardoso et al. [10] found no significant difference in this biomarker between RAS and controls.
The present work demonstrated elevated levels of SAA in ulcerative phase compared to post-healing phase. Opposite to our findings, Piceck et al. [26] have measured SAA levels in patients with RAS during acute phase and remission period, and found that these levels were increased during remission period (i.e., when patients did not have ulcerations in the mouth) compared to the period when they had ulcerations in the oral cavity. Activity of SAA might reflect catecholamine serum levels in various stress situations. Elevated SAA is a short-lived response, owing to reflex ANS [20]. However, Vineetha et al. [22] found that SAA activity increases in patients with chronic psychosocial stress and may be used as a biomarker of chronic stress.
We postulate that the presence of a high level of the salivary stress biomarkers in the post-healing phase in comparison to the control group can indicate that the patients with RAS might have chronic stress or anxiety.
The present study demonstrated a strong positive correlation between levels of cortisol and amylase in the post-healing phase, whereas this correlation was insignificant in the ulcerative phase. The ANS and HPA axis are known to cooperatively function in normal conditions, having parallel up-regulations. The absence of correlation in the ulcerative phase is in accordance with Takai et al. [27] who found that SC levels showed lesser extent of increase when compared to SAA after the induction of a stressor. The latency time to peak level for cortisol was longer than that of amylase. They concluded that SAA serves as a better index of acute stress. A similar finding was also reported by other investigators [28]. On the other hand, the presence of a positive correlation of both biomarkers in the post-healing phase might give more proof of the role of chronic anxiety and/or stress in patients with RAS.
The small sample size is the main limitation of this study and further work with a larger number of patients is warranted to further verify the findings of the current work.
Conclusion
From the present study, it could be concluded that RAS patients have high SC and SAA levels, the stress biomarkers, denoting a potential role of stress in the etiopathogenesis of RAS. In addition, the high levels of these biomarkers in the healing-phase of RAS can point to a possible role of chronic stress and anxiety among the patients suffering from RAS. Further studies are needed to better clarify the existence of chronic stress and anxiety in these patients.
Conflict of interest
The authors declares that they have no conflicts of interest in relation to this article.
Funding
This project was supported by Deanship of Scientific Research (DSR) at King Abdulaziz University, Jeddah, Saudi Arabia (Project No. 516/165/1435).
Ethical approval
This study has been approved by the Research Ethics Committee of the Faculty of Dentistry, King Abdul Aziz University.
Informed consent
Written informed consent was obtained from everyone involved in this study.
Authors contribution
– Ghada Mansour: Research idea, data collection, analysis of results, reference collection, manuscript writing, final manuscript revision. – Khalid Aljohani: Research idea, data collection, reference collection, final manuscript revision. – Mohammad-Ayman Safi: Laboratory work, analysis of results. – Late Prof. Soliman Ouda: Research idea, data collection, reference collection.
Acknowledgements
This project was supported by Deanship of Scientific Research (DSR) at King Abdulaziz University, Jeddah, Saudi Arabia (Project No. 516/165/1435). The authors, therefore, acknowledge with thanks DSR technical and financial support. We would like also to acknowledge the late professor Soliman Ouda, (Department of Oral Diagnostic Sciences, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia) for his valuable contribution in the proposal, practical part, and manuscript preparation.
References
- Kaur R, Behl AB, Punia RS, Nirav K, Singh KB, Kaur S. Assessment of prevalence of recurrent aphthous stomatitis in the north Indian population: a cross-sectional study. J Pharm Bioallied Sci 2021; 13:S363– S366. [CrossRef] [PubMed] [Google Scholar]
- Akintoye SO, Greenberg MS. Recurrent aphthous stomatitis. Dent Clin North Am 2005;49:31–47. [CrossRef] [PubMed] [Google Scholar]
- Queiroz S, Silva, M, Medeiros A, Oliveira PT, Gurgel B, Silveira É. Recurrent aphthous ulceration: An epidemiological study of etiological factors, treatment, and differential diagnosis. An Bras Dermatol 2018;93:341–346. [CrossRef] [PubMed] [Google Scholar]
- Gallo Cde B, Mimura MA, Sugaya NN. Psychological stress and recurrent aphthous stomatitis. Clinics (Sao Paulo) 2009;64:645–648. [CrossRef] [Google Scholar]
- Suresh KV, Shenai P, Chatra L, Ronad YA, Bilahari N, Pramod RC, et al. Oral mucosal diseases in anxiety and depression patients: hospital based observational study from south India. J Clin Exp Dent 2015;7:e95–e99. [CrossRef] [PubMed] [Google Scholar]
- Phillips LJ, McGorry PD, Garner B, Thompson KN, Pantelis C, Wood SJ, et al. Stress, the hippocampus and the hypothalamic-pituitary-adrenal axis: implications for the development of psychotic disorders. Aust N Z J Psychiatry 2006;40:725–741. [CrossRef] [PubMed] [Google Scholar]
- Rezaei F, Aminian M, Raygani AV. Evaluation of salivary cortisol changes and psychological profiles in patients with recurrent aphthous stomatitis. Contemp Clin Dent. 2017;8:259–263. [CrossRef] [PubMed] [Google Scholar]
- Nadendla LK, Meduri V, Paramkusam G, Pachava KR. Relationship of salivary cortisol and anxiety in recurrent aphthous stomatitis. Indian J Endocrinol Metab 2015;19:56–59. [CrossRef] [PubMed] [Google Scholar]
- Kunikullaya UK, Kumar MA, Ananthakrishnan V, Jaisri G. Stress as a cause of recurrent aphthous stomatitis and its correlation with salivary stress markers. Chin J Physiol 2017;60:226–230. [CrossRef] [PubMed] [Google Scholar]
- Cardoso JA, Dos Santos Junior AA, Nunes ML, de Figueiredo MA,Cherubini K, Salum FG. Salivary alpha-amylase enzyme, psychological disorders, and life quality in patients with recurrent aphthous stomatitis. Int J Dent 2017;2017:5269856. [PubMed] [Google Scholar]
- Al-Johani K. Prevalence of recurrent aphthous stomatitis among dental students: a cross sectional study. J Contemp Dent Pract 2019;20:893–895. [CrossRef] [PubMed] [Google Scholar]
- Soto Araya M, Rojas Alcayaga G, Esguep A. Association between psychological disorders and the presence of oral lichen planus, burning mouth syndrome and recurrent aphthous stomatitis. Med Oral 2004;9:1–7. [PubMed] [Google Scholar]
- McCartan BE, Lamey PJ, Wallace AM. Salivary cortisol and anxiety in recurrent aphthous stomatitis. J Oral Pathol Med 1996;25:357–359. [CrossRef] [PubMed] [Google Scholar]
- Albanidou-Farmaki E, Poulopoulos AK, Epivatianos A, Farmakis K, Karamouzis M, Antoniades D. Increased anxiety level and high salivary and serum cortisol concentrations in patients with recurrent aphthous stomatitis. Tohoku J Exp Med 2008;214:291–296. [CrossRef] [PubMed] [Google Scholar]
- Huling LB, Baccaglini L, Choquette L, Feinn RS, Lalla RV. Effect of stressful life events on the onset and duration of recurrent aphthous stomatitis. J Oral Pathol Med 2012;41:149–152. [CrossRef] [PubMed] [Google Scholar]
- Pedersen A. Psychologic stress and recurrent aphthous ulceration. J Oral Pathol Med 1989;18:119–122. [CrossRef] [PubMed] [Google Scholar]
- Susanto H, Kendarwati P, Imanusti K, Widyanigsih L. Decreased salivary cortisol in recurrent aphthous stomatitis treated with topical steroids. J Islam Dent Assoc Iran 2019;31:26–32. [CrossRef] [Google Scholar]
- Shirasaki S, Fujii H, Takahashi M, Sato T, Ebina M, Noto Y, et al. Correlation between salivary alpha-amylase activity and pain scale in patients with chronic pain. Reg Anesth Pain Med 2007; 32:120–123. [CrossRef] [PubMed] [Google Scholar]
- Lisa Cheng YS, Jordan L, Gorugantula LM, Schneiderman E, Chen HS, Rees T. Salivary interleukin-6 and −8 in patients with oral cancer and patients with chronic oral inflammatory diseases. J Periodontol 2014;85:956–965. [CrossRef] [PubMed] [Google Scholar]
- Rutherfurd-Markwick K, Starck C, Dulson DK, Ali A. Salivary diagnostic markers in males and females during rest and exercise. J Int Soc Sports Nutr 2017;14:27. [CrossRef] [PubMed] [Google Scholar]
- Safarzadeh E, Mostafavi F, Haghi-Ashtiani MT. Determination of salivary cortisol in healthy children and adolescents. Acta Med Iran 2005;43:32–36. [Google Scholar]
- Vineetha R, Pai KM, Vengal M, Gopalakrishna K, Narayanakurup D. Usefulness of salivary alpha amylase as a biomarker of chronic stress and stress related oral mucosal changes − a pilot study. J Clin Exp Dent 2014;6:e132–e137. [CrossRef] [PubMed] [Google Scholar]
- Zakaria M, Hosny R. Relation between salivary cortisol and alpha amylase levels and anxiety in Egyptian patients with minor recurrent aphthous stomatitis. Egypt Dent J 2018;64:1235–1243. [CrossRef] [Google Scholar]
- Nurdiana N, Ritonga PWU, Wulandari P. The role of stress in recurrent aphthous stomatitis. Eur J Gen Dent 2023;12:42–47. [Google Scholar]
- Vandana S, Kavitha B, Sivapathasundharam B. Salivary cortisol and dehydro-epiandrosterone as oral biomarkers to determine stress in patients with recurrent aphthous stomatitis. J Oral Maxillofac Pathol 2019;23:213–217. [CrossRef] [PubMed] [Google Scholar]
- Picek P, Rogulj AA, Boras VV, Stipetić-Ovcarićek J, Catić A, Plestina S, et al. Serum and salivary parameters in patients with recurrent aphthous ulcerations. Acta Stomatolo Croatica 2012; 46:43–49. [Google Scholar]
- Takai N, Yamaguchi M, Aragaki T, Eto K, Uchihashi K, Nishikawa Y. Effect of psychological stress on the salivary cortisol and amylase levels in healthy young adults. Arch Oral Biol 2004;49:963–968. [CrossRef] [PubMed] [Google Scholar]
- Ali N, Nater UM. Salivary alpha-amylase as a biomarker of stress in behavioral medicine. Int J Behav Med 2020;3:1–6. [Google Scholar]
All Tables
Comparison of salivary Alpha amylase and salivary cortisol between control group and RAS patients during the ulcerative and post-healing phases.
All Figures
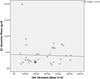 |
Fig. 1 Graph showing correlation between SAA and SC in the ulcerative phase. |
| In the text | |
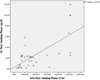 |
Fig. 2 Graph showing correlation between SAA and SC in the post-healing phase. |
| In the text | |
Current usage metrics show cumulative count of Article Views (full-text article views including HTML views, PDF and ePub downloads, according to the available data) and Abstracts Views on Vision4Press platform.
Data correspond to usage on the plateform after 2015. The current usage metrics is available 48-96 hours after online publication and is updated daily on week days.
Initial download of the metrics may take a while.


